How Do Rheumatoid And Osteoarthritis Differ?
Author: Dr. Stephen Chaney
 This week I am concluding my series on recent omega-3 advances by reviewing a meta-analysis that asks whether omega-3s are beneficial for people with osteoarthritis.
This week I am concluding my series on recent omega-3 advances by reviewing a meta-analysis that asks whether omega-3s are beneficial for people with osteoarthritis.
This is an important question because osteoarthritis affects around 32.5 million adults in the United States, and that number is increasing each year as our population ages. Osteoarthritis causes pain and disabilities that can significantly affect quality of life.
And the costs are high. Health care costs due to osteoporosis are around $140 billion/year. And when you include lost workdays, the annual cost is around $468 billion.
There are several medications for reducing symptoms of osteoarthritis. But they each have side effects and some patients cannot tolerate them. Joint replacement surgery is the final resort. But the recovery period is long, and the surgery isn’t always effective. For both reasons many patients with osteoarthritis are looking for natural solutions.
Most of the research on omega-3s and arthritis has been done with patients who have rheumatoid arthritis. Omega-3 supplements have been shown to reduce the pain, swelling of the joints, and inflammation associated with rheumatoid arthritis for many people with the disease.
Based on several dose-response studies, the NIH says the optimal dose is around 2.7 gm/day of EPA + DHA but cautions not to go above 3 gm/day without your doctor’s OK.
The evidence is less clear for omega-3s and osteoarthritis. Some studies suggest that EPA + DHA reduce the pain and inflammation associated with osteoarthritis. But other studies have come up empty. There is no consensus as to whether omega-3s are beneficial for people with osteoarthritis.
When there is disagreement between individual studies, a meta-analysis of the studies is often helpful. By pooling the data from multiple studies, a meta-analysis can smooth out some of the differences between the studies and accumulate enough data points to discover effects that would not have been statistically significant with the smaller data sets from individual studies.
With that in mind, the authors of this manuscript (W Den et al, Journal of Orthopaedic Surgery and Research, 18: 381, 3023) performed a meta-analysis on the data obtained from 9 double-blind, placebo-controlled studies looking at the effect of omega-3s versus a placebo on both pain and joint mobility in osteoarthritis patients.
How Do Rheumatoid And Osteoarthritis Differ?
 While the causes of rheumatoid arthritis and osteoarthritis are very different, there are some underlying similarities between the two diseases that suggest both might benefit from omega-3 supplementation.
While the causes of rheumatoid arthritis and osteoarthritis are very different, there are some underlying similarities between the two diseases that suggest both might benefit from omega-3 supplementation.
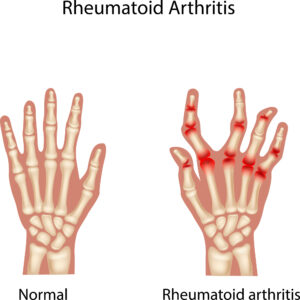
Rheumatoid Arthritis: Rheumatoid arthritis is thought to be an autoimmune disease, which means that our immune system attacks our cells rather than foreign invaders. It results in chronic inflammation that attacks our joints and can affect other tissues in our body.
It initially affects the lining of our joints which can result in painful, swollen joints. As the disease progresses it can also lead to bone erosion and joint deformity.
Osteoarthritis: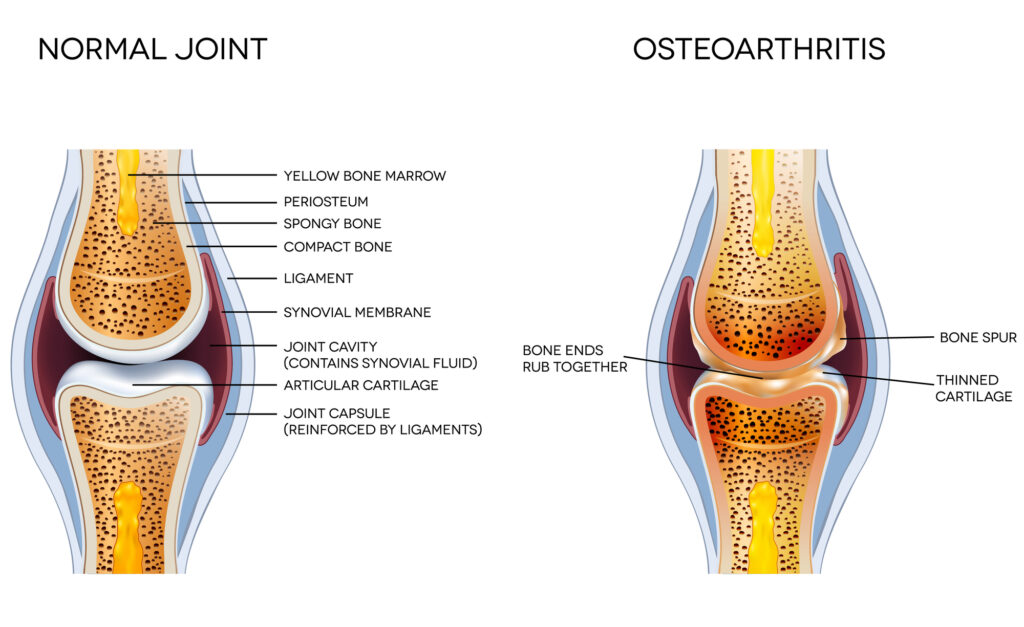 Osteoarthritis is generally thought of as a “wear and tear” disease. It is associated with sports injuries and accidents. It is also associated with stress to particular joints due to repeated motions associated with either sports or a job. Obesity also increases wear and tear of the joints because it increases the load on the joints.
Osteoarthritis is generally thought of as a “wear and tear” disease. It is associated with sports injuries and accidents. It is also associated with stress to particular joints due to repeated motions associated with either sports or a job. Obesity also increases wear and tear of the joints because it increases the load on the joints.
The wear and tear causes the cartilage that cushions the junction between bones to deteriorate. Eventually, the cartilage deteriorates to the extent that bone is grinding against bone, which can lead to bone loss and deformities.
Eventually, this results in an inflammation of the joint lining which causes pain and accelerates bone loss. It also causes deterioration of the connective tissue which holds bones together and connects them to muscle.
What Do These Diseases Have In Common? Inflammation is the common factor associated with both rheumatoid and osteoarthritis, and many studies suggest that omega-3s reduce inflammation. In the simplistic description of the two diseases I shared above, it sounds like inflammation occurs much earlier in the disease process for rheumatoid arthritis than for osteoarthritis. This might suggest that omega-3s could be more effective at reducing the symptoms and progression of rheumatoid arthritis than of osteoarthritis.
However, we know that the risk of developing osteoarthritis is increased by chronic inflammation caused by obesity, diseases like diabetes, and/or an inflammatory diet.
How Was This Study Done?
 This study was a meta-analysis of 9 double-blind, placebo-controlled clinical studies looking at the effect of omega-3 fatty acids on the pain and loss of joint mobility associated with osteoarthritis. These studies were performed in countries from around the world and included a total of 2,070 participants.
This study was a meta-analysis of 9 double-blind, placebo-controlled clinical studies looking at the effect of omega-3 fatty acids on the pain and loss of joint mobility associated with osteoarthritis. These studies were performed in countries from around the world and included a total of 2,070 participants.
The criteria for inclusion in the meta-analysis were:
1) The articles were written in English.
2) The studies had to be double-blind, placebo-controlled studies (The gold standard for clinical studies).
3) Patients with osteoarthritis were randomly assigned to an intervention group receiving omega-3 supplementation or a placebo group receiving olive oil or another plant oil.
4) The studies measured efficacy and safety outcomes including joint pain (efficacy), joint mobility (efficacy), and treatment-related adverse events (safety).
5) Patients in both the omega-3 and placebo groups were using medications to reduce osteoarthritis symptoms when they were enrolled in the study and were advised to continue with their prescribed medicines for the duration of the study.
The characteristics of the clinical studies included in this meta-analysis were:
- Sample size (47-1221), Average = 230.
- Mean age (55.9-68), Average = 63.
- % men (13.8-45.1%), Average = 31%.
- Omega-3 (EPA + DHA) dose (350 mg/day – 2,400 mg/day), Average = 1,085 mg/day.
Do Omega-3s Reduce Osteoarthritis Pain?
 When the data from all 9 studies were combined in a single meta-analysis, omega-3 (EPA + DHA) supplementation:
When the data from all 9 studies were combined in a single meta-analysis, omega-3 (EPA + DHA) supplementation:
- Reduced joint pain by 29% compared to the placebo.
- Increased joint mobility by 21% compared to the placebo.
- Was not associated with any adverse effects.
The authors concluded, “The results of the meta-analysis indicate that supplementation with omega-3 fatty acids is effective to relieve pain and improve joint function in patients with osteoarthritis, without increasing the risk of treatment-related adverse events. These findings support the use on omega-3 fatty acid supplementation as an alternative treatment for osteoarthritis.”
What Are The Strengths and Limitations Of This Study?
- All the studies included in this meta-analysis were randomized, double-blind, placebo-controlled studies (the gold standard for clinical trials).
- All the individual studies that qualified for this meta-analysis found that omega-3 supplementation reduced joint pain and improved joint mobility. This improves confidence that the conclusions of the meta-analysis are correct. The meta-analysis simply improved the statistical significance of this conclusion by combining the data from the individual studies.
Limitations:
- The biggest limitation was that the individual studies included in this meta-analysis were not performed under the guidelines of the “Fatty Acids and Outcomes Research Consortium” that I discussed in last week’s issue of “Health Tips From the Professor”.
-
- The “Fatty Acids and Outcomes Research Consortium” guidelines harmonize the designs of individual studies, which strengthens the meta-analysis.
-
-
- In contrast, the design of the individual studies within this meta-analysis was very different, which prevented the meta-analysis from being able to determine the optimal dose of omega-3 supplements and the minimum time required for omega-3 supplementation to significantly reduce the symptoms of osteoarthritis.
-
-
- The “Fatty Acids and Outcomes Research Consortium” guidelines would have also required these studies to measure tissue levels of omega-3s (something called Omega-3 Index) at the beginning and end of each study. This was not done in any of these studies.
-
-
- This is important because if a patient’s tissue levels of omega-3s at the beginning of the study were already in the optimal range, you would expect little additional benefit from supplementation for that patient.
-
- All the individual studies were very small. This limits the ability of these studies to provide definitive conclusions. Unfortunately, this is probably unavoidable.
-
- Double blind, placebo-controlled clinical studies are expensive. Only major pharmaceutical companies have the multi-million-dollar budgets required to conduct large double blind, placebo-controlled clinical studies that would provide more definitive evidence that omega-3 supplementation reduces the symptoms of osteoarthritis – and the follow-up studies that would determine the optimal dose of omega-3 supplements and the minimum time required to show an effect of omega-3 supplementation.
- The patients in these studies were already taking medications to reduce their osteoarthritis symptoms prior to entering the study and were instructed to continue taking those medications during the study. This means that the studies were not asking whether omega-3s alone were effective at reducing osteoarthritis symptoms. They were asking whether omega-3 supplementation provided any additional benefits for people who were already taking medications to reduce symptoms.
-
- Unfortunately, this is also probably unavoidable. Current guidelines consider it unethical to withhold the medical “standard of care” from any patient in a clinical trial.
What Does This Study Mean For You?
 This study, while not definitive, strengthens the evidence that omega-3 supplements containing EPA + DHA may reduce joint pain and improve joint mobility for people with osteoarthritis. It also shows that the doses required to achieve these benefits are not associated with any significant side effects.
This study, while not definitive, strengthens the evidence that omega-3 supplements containing EPA + DHA may reduce joint pain and improve joint mobility for people with osteoarthritis. It also shows that the doses required to achieve these benefits are not associated with any significant side effects.
While large scale double blind, placebo-controlled clinical studies to confirm these conclusions would be nice, they are unlikely to occur for the reasons discussed above.
The investigators said, “[This study shows that] supplementation of omega-3 fatty acids is effective to relieve pain and improve joint function in patients with osteoarthritis…These findings support the use of omega-3 fatty acid supplementation as an alternative treatment for osteoarthritis.”
This might lead you to believe that omega-3 fatty acids can potentially replace medications for reducing osteoarthritis pain and loss of joint mobility. That may be true, but that is not what the study showed.
Patients in both the omega-3 and placebo group continued their prescribed medicines for osteoarthritis. In reality, the study only shows that omega-3s provide additional benefit for people already taking osteoarthritis medications. The effect of omega-3 supplements by themselves has not been tested and, as I discussed above, is not likely to be tested in the foreseeable future.
However, the use of omega-3 supplements may allow you to reduce or eliminate the medications you are on for osteoarthritis and may delay the need for joint replacement surgery. Of course, if you wish to reduce/eliminate your medications and/or delay joint replacement surgery, I recommend consulting with your doctor first.
Finally, this study provides no information on the optimal dose of omega-3s. Some studies suggest the dose of omega-3s needed to reduce osteoarthritis symptoms may be less than that required to reduce rheumatoid arthritis symptoms, but that evidence is weak.
In the absence of good dose response data, I recommend you aim for an omega-3 index of 8%. You will find a more detailed discussion of the Omega-3 Index and how to use it in last week’s “Health Tips From the Professor” article .
The Bottom Line
A recent meta-analysis looked at the effect of omega-3 supplementation on the pain and lack of joint mobility associated with osteoarthritis.
The study showed that omega-3 (EPA + DHA) supplementation:
- Reduced joint pain by 29% compared to the placebo.
- Increased joint mobility by 21% compared to the placebo.
- Was not associated with any adverse effects.
The authors concluded, “The results of the meta-analysis indicate that supplementation with omega-3 fatty acids is effective to relieve pain and improve joint function in patients with osteoarthritis, without increasing the risk of treatment-related adverse events.”
For more details about the study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.