Would You Like To Be A Guinea Pig?
Author: Dr. Stephen Chaney
 Peptide stacks are all latest “magic” weight-loss potion. If you watch social media, the hype is hard to escape. If you believe the promises:
Peptide stacks are all latest “magic” weight-loss potion. If you watch social media, the hype is hard to escape. If you believe the promises:
- The weight will magically melt away.
- Fat will disappear and be replaced with muscle.
- You’ll have the energy to leap tall buildings in a single bound.
- Aches & pains will disappear.
And that’s just the tip of the iceberg. What’s not to like?
Let’s start at the beginning. Peptide stacks are simply multiple peptide hormones with different benefits that are given as a single injection – usually once or twice a day.
To help you understand their benefits and risks, I will discuss:
- Metabolism 101: How Do Peptide Hormones Work?
- The Allure of Peptide Stacks.
- GLP-1 Drugs: A Cautionary Tale
- Are Peptide Stacks Safe?
- Would You Like To Be A Guinea Pig?
Metabolism 101: How Do Peptide Hormones Work?
Peptide hormones are short chains of amino acids, usually 10 to 100 amino acids in length. You can think of them as short proteins. In fact, many peptide hormones start out as a larger precursor protein that is cleaved into several different peptide hormones.
- Peptide hormones are released from specific cells in response to a physiological signal.
- They bind to target tissues and produce an effect on metabolism, growth, or reproduction.
- Once they have achieved the desired effect and the original physiological signal disappears, they are rapidly degraded and replaced by different peptide hormones that often have the opposite effect.
But that simplistic description just scratches the surface.
- Sometimes they act like a cross between a “bucket brigade” and a spider web.
 Regulation of human growth hormone (HGH) is an example.
Regulation of human growth hormone (HGH) is an example.
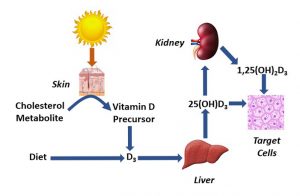
- Fasting caused the stomach to release the peptide hormone ghrelin, which stimulates the hypothalamus to release growth hormone releasing factor (HGRF). Low blood glucose, which is associated with fasting, also causes the hypothalamus to release HGRF.
- Sleep, especially the early stages of deep sleep, also stimulates the hypothalamus to release HGRF.
- HGRF binds to the pituitary and stimulates it to release HGH. HGH binds to nearly every tissue and organ in the body and has multiple effects. I’ll just mention a few of them here. For example,
- HGH binds to the liver and causes it to release insulin-like growth factor-1 (IGF-1).
- IGF-1 opposes the effect of insulin. It causes the liver to release glucose into the bloodstream and the liver and other tissues to release fat into the bloodstream. This helps the body get the energy it needs during the fasting state. It also provides the energy needed for growth.
- It also stimulates the growth of muscle and bone. This is part of the growth response to HGH.
- And, of course, all these responses support tissue repair, metabolism, and growth during sleep.
These effects of HGH are short-lived. HGH is meant to be released in short pulses as needed by the body. Once the desired effects of HGH have been realized, its production is stopped and it is rapidly degraded.
- IGF-1 and/or high levels of blood glucose and fatty acids cause the hypothalamus to halt production of GHRF and release a peptide hormone called somatostatin instead.
- Somatostatin binds to the pituitary and blocks the release of HGH.
This description is a simplistic view of the effects and regulation of HGH. Ghrelin, HGH and IGF-1 each have multiple other targets within the body. They influence multiple metabolic reactions. And both HGH and IGF-1 are regulated by other peptide hormones, each responding to different physiological stimuli.
So, you can see where my analogy of a bucket brigade and spider web came from.
- The bucket brigade is: stomach → ghrelin → hypothalamus → GHRF → pituitary → HGH → liver → IGF-1
- The spider web is the multiple other targets of ghrelin, HGH, and IGF-1 and the other peptide hormones that stimulate the release HGH and IGF-1.
But the analogy of a bucket brigade and spider web is a static representation. Each peptide hormone is constantly changing over time. Perhaps a better analogy would be an intricate dance, with dance partners constantly changing, disappearing, and reappearing.
When I look at the intricacies of metabolic regulation it seems inescapable that there must be a divine creator. This could not have happened by chance. And metabolic regulation is just one aspect of the amazing human body.
The Allure Of Peptide Stacks
 When I think of the allure of peptide stacks, the image that comes to mind is the sirens of Greek Mythology. They were variously described as bird-like or mermaid-like creatures who sat on the shoreline and sang such enchanting songs that they lured sailors to their deaths on the rocky shoals just off the coast.
When I think of the allure of peptide stacks, the image that comes to mind is the sirens of Greek Mythology. They were variously described as bird-like or mermaid-like creatures who sat on the shoreline and sang such enchanting songs that they lured sailors to their deaths on the rocky shoals just off the coast.
In Homer’s Odyssey, he wrote about Ulysses putting earplugs in his crew and tying himself to the mast, so they could safely pass by the sirens without being lured to their death.
In this section, I will talk about the allure of peptide stacks. I’ll discuss the rocks later.
Perhaps the best way to talk about the allure of peptide stacks is to give specific examples of some of the most popular peptides included in the stacks.
Tesamorelin is a synthetic analog of growth hormone releasing factor (GHRF) that stimulates the pituitary to release growth hormone (HGH), which stimulates the liver to release insulin-like growth factor-1 (IGF-1).
- It is associated with muscle growth and fat loss, especially abdominal fat.
Ipamorelin is a synthetic peptide that mimics the effects of ghrelin. In short, it stimulates the hypothalamus to release GHRF, which stimulates the pituitary to release HGH, which stimulates the liver to release IGF-1.
- It is associated with muscle growth, fat loss, recovery and healing.
CJC-1295 is another synthetic analog of GHRH.
- It is associated with muscle growth, fat loss, improved recovery and healing, increased energy, and better bone density.
AOD-9604 is a synthetic analog of HGH. However, it is only a portion of the HGH molecule. It promotes weight loss but does not increase muscle mass or help with blood sugar control.
BPC-157 is a synthetic analog of a peptide found in gastric juice.
- It is associated with wound healing, gastrointestinal health, and reduced inflammation.
TB-500 is a synthetic analog of thymosin-beta-4, a peptide released by platelets, macrophages, and smooth muscle cells after injury.
- It is associated with accelerated wound healing, reduced inflammation, increased flexibility and mobility, and muscle growth.
Tirzepatide is a synthetic analog of GLP-1. Like other GLP-1 it improves blood sugar control and suppresses appetite, which can lead to significant weight loss.
- The FDA approved version of tirzepatide is sold under the trade names Mounjaro and Zepbound. However, the tirzepatide you find in peptide stacks is neither FDA approved nor FDA regulated. I will discuss what the FDA says about this below.
Of course, the “magic” of peptide stacks is that several of these peptides are combined in each injection, so you are maximizing the health “benefits”.
And when you look at the claimed health benefits – weight loss, fat loss, muscle growth, reduced inflammation, energy, improved flexibility, and much more – the allure of peptides stacks is easy to understand.
But is there a downside to peptide stacks? It’s time to examine the rocks along the shoreline. But first I should share a cautionary tale about GLP-1 drugs because that helps us understand the potential problems with peptide stacks.
GLP-1 Drugs – A Cautionary Tale
 GLP-1 is a peptide secreted by specialized cells in the intestine every time we have a meal.
GLP-1 is a peptide secreted by specialized cells in the intestine every time we have a meal.
- It activates satiety cells in our brain to tell us we are full and don’t need to eat any more.
- It also slows the emptying of our stomach and slows the transit time of food in our intestine. That helps us maximize the absorption of nutrients from our meal. It also prolongs the physical feeling of fullness.
But this effect only lasts an hour or two. Soon GLP-1 is broken down, and other peptide hormones take over to keep nutrient levels steady in the bloodstream and prepare us for the next meal. This is part of that “intricate dance” of peptide hormones that I described earlier.
Some bright scientists working for pharmaceutical companies hypothesized that if GLP-1 levels remained high for days rather than hours they could achieve long-term appetite suppression, which would help with weight loss. They created synthetic versions of GLP-1 drugs which were stable in the bloodstream for up to a week and injected them into patients at levels 10 to 100 times higher than found in nature.
Because these drugs were developed by pharmaceutical companies, they went through the complete FDA approval and inspection process. This involves:
- Double-blind, placebo-controlled clinical studies with hundreds of patients establishing that the drugs are safe and effective. These studies are of the quality that they are published in peer-reviewed scientific journals.
- Careful review of the clinical studies by the FDA as part of the approval process.
- Regular inspection of the drug production facilities by the FDA to assure adherence to the highest quality and purity standards.
- Post-Market monitoring after approval to identify any safety concerns that were missed in the approval process. Doctors and pharmaceutical companies are required to report any serious side effects to the FDA.
-
- During the approval process the drugs are tested in hundreds of patients. After approval the drugs are often used by millions of patients. Also, some side effects are cumulative and do not appear until the drugs have been used for a long time. It is not unusual to identify serious side effects through this post-marketing monitoring process.
Some of the side effects were predictable and were discovered in the original clinical trials of these drugs.
- Because the GLP-1 analogs are present at higher levels and for much longer than natural GLP-1, stomach emptying and transit times through the intestine were delayed much more than normal.
-
- This results in side effects like nausea, vomiting, diarrhea, constipation, bloating, and stomach pain.
However, some of the most-concerning side effects were only discovered through the post-marketing review process. These include.
- Increased anxiety, depression, and suicidal thoughts. These side effects, especially suicidal thoughts, are of concern to anyone who already experiences some degree of anxiety and/or depression.
- Loss of muscle mass. This is of concern to adults over the age of 50 because many of them already suffer from sarcopenia (age-related muscle loss).
Why is this a cautionary tale, you might ask? It’s cautionary because the common side effects and the more serious side effects for GLP-1 drugs were only discovered because of the FDA drug approval and post-marketing review procedures. Spoiler alert: None of the peptide stacks have gone through this kind of review process.
Are Peptide Stacks Safe?
 The question I posed at the beginning of this article is, “Are peptide stacks safe?” The short answer is, “We don’t know but there are several reasons to be cautious”.
The question I posed at the beginning of this article is, “Are peptide stacks safe?” The short answer is, “We don’t know but there are several reasons to be cautious”.
#1: Peptide hormones are not natural (And it’s not nice to fool around with Mother Nature).
Specifically, the dosage and timing of peptide stacks is not natural. In my overview of peptide hormones, I talked about the “intricate dance” peptide hormones undergo as they control human metabolism.
In short, peptide hormones are under tight control by our bodies. They are produced in the right amount, at the right time, and for the right duration (They are degraded as soon as they have completed their mission). None of this is true for peptide stacks.
- They are injected on a fixed schedule – not when our bodies need them (not the right time).
- They are injected at doses designed to create much higher blood levels than the body produces under normal circumstances (not the right amount).
- They are injected with frequencies designed to achieve high blood levels far longer than seen under normal circumstances (not the right duration).
And if we have learned anything from GLP-1 drugs, it is that when we create synthetic peptide hormones and inject them at the wrong time, at the wrong amount, and for the wrong duration we create side effects and some of those side effects may have significant health consequences.
#2: We have no idea whether peptide stacks are effective and safe. These are not FDA approved treatments. That means:
- No human clinical trials have been performed to assess efficacy and safety of peptide stacks.
- There is no post-marketing monitoring. Simply put, that means there is no system in place to monitor the frequency and severity of side effects.
#3: We have no idea whether peptide stacks are pure and potent. They are typically produced by compounding pharmacies or overseas manufacturers who may not use good manufacturing practices and quality controls.
The FDA has recently released a warning about one of these synthetic peptide hormones (tirzepatide) produced by compounding pharmacies and overseas manufacturers and available online. Their findings were that some of the samples they evaluated:
- Had inaccurate label information.
- Contained too little, too much, or no active ingredient at all.
- Contained the wrong ingredients.
- Contained harmful contaminants.
While this report focused on a single peptide, there is no reason to suspect that compounding pharmacies and overseas manufacturers would do a better job of producing other synthetic peptide hormones.
In short, it is buyer beware in the online peptide stack marketplace.
Would You Like To Be A Guinea Pig?
 To sum up the previous section:
To sum up the previous section:
- Peptide stacks are not natural. This may result in unexpected side effects.
- There are no published human clinical studies on peptide stacks. That means:
- We have no idea whether they are safe and effective. There is no evidence that the claimed benefits are true, and we don’t know what the side effects might be.
- No one is monitoring the manufacturing practices and quality controls for peptide stacks. That means:
-
- We have no idea whether they are pure and potent. We don’t know how much of each peptide hormone they contain and whether the hormones are pure.
In short, using the peptide stacks currently available online is like volunteering to be a guinea pig in a long-term clinical trial with an uncertain outcome.
Now I know many of you prefer to go outside of the medical system, and it may seem to you that I am taking the side of the FDA and pharmaceutical companies.
That is not the case. I do get regular checkups, but my doctor is fully aware that I prefer natural approaches whenever possible. I’m 81, use no medications, and am in excellent health.
I choose natural approaches that are proven to be safe and effective. Peptide stacks are not there yet. I choose not to be a guinea pig.
But if the allure of peptide stacks still tempts you, the best advice I have seen is to work with licensed health professionals.
- They normally research their sources and know which companies use good manufacturing practices and perform rigorous quality controls on their products.
-
- It’s your responsibility to ask them how they choose which products they recommend.
- They normally monitor you for side effects.
-
- It’s your responsibility to ask them how they want to monitor you for side effects and to report any side effects to them as soon as you notice them.
The Bottom Line
Peptide stacks are the latest “magic” weight-loss potion. When I think of the allure of peptide stacks, the image that comes to mind is the sirens of Greek Mythology. They were variously described as bird-like or mermaid-like creatures who sat on the shoreline and sang such enchanting songs that they lured sailors to their deaths on the rocky shoals just off the coast.
In this article I describe their allure. I also describe the rocky shoals.
- Peptide stacks are not natural. This may result in unexpected side effects.
- There are no published human clinical studies on peptide stacks. That means:
-
- We have no idea whether they are safe and effective. There is no evidence that the claimed benefits are true, and we don’t know what the side effects might be.
- No one is monitoring the manufacturing practices and quality controls for peptide stacks. That means:
-
- We have no idea whether they are pure and potent. We don’t know how much of each peptide hormone they contain and whether the hormones are pure.
In short, using the peptide stacks currently available online is like volunteering to be a guinea pig in a long-term clinical trial with an uncertain outcome.
For more information on peptide stacks and the best recommendations if you choose to use them, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 54 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.