What Does This Mean For You?
Author: Dr. Stephen Chaney
 You may remember the nursery rhyme, “Jack Sprat could eat no fat. His wife could eat no lean…” You may know people who fit these extremes. And in terms of diets these extremes might represent the vegan and keto diets in today’s world.
You may remember the nursery rhyme, “Jack Sprat could eat no fat. His wife could eat no lean…” You may know people who fit these extremes. And in terms of diets these extremes might represent the vegan and keto diets in today’s world.
The nursery rhyme assures us that, “…between them they licked the platter clean.” But were their diets equally healthy? Which of them would have been more likely to live a long and healthy life?
And, since this is Heart Health Month, we might ask, “Which diet would have been better for their hearts?”
If you search Mr. Google – even with AI assist – you might be confused. That’s because AI bases its recommendations on the quantity of posts, not the accuracy of posts. And lots of media influencers recommend both diets, and just about every popular diet in between for heart health.
But what does good science say on the topic of heart healthy diets? Fortunately, a recent comprehensive review and meta-analysis (G. Riccardi et al, Cardiovascular Research, 118: 1118-1204, 2022) has answered that question.
How Was The Study Done?
 The investigators reviewed 99 clinical studies with tens of thousands of participants that looked at the associations between foods or food groups and heart disease risk.
The investigators reviewed 99 clinical studies with tens of thousands of participants that looked at the associations between foods or food groups and heart disease risk.
Most of the studies were “prospective cohort” studies in which:
- Populations are divided into groups (cohorts) based on the foods they consume…
- …and followed for a number of years (this is where the term “prospective” comes from)…
- …and at the end of the study, the association between food and heart outcomes is measured.
However, the review also included several major randomized controlled clinical trials, including:
- The DASH diet study.
- The Lyon Diet Heart study.
- The PREDIMED study.
Eating For A Healthy Heart
 Here are the findings of the study. Most will sound very familiar. But you will note some subtle differences based on recent data.
Here are the findings of the study. Most will sound very familiar. But you will note some subtle differences based on recent data.
The overall summary was that for a healthy adult population:
- Low consumption of salt and foods of animal origin…
- …and increased intake of plant foods…
- …are associated with reduced heart disease risk.
Of course, we have known that for years. It’s when they broke the data down further that it became more interesting.
Foods Of Animal Origin:
- Processed meats increase heart disease risk. A single serving of processed meat is associated with a 27% to 44% increased risk of heart disease. This is not new.
- Unprocessed red meat is also associated with increased risk of heart disease, but this association is not as
 consistent as for processed meats. The authors noted that some of this may be due to differences in saturated fat content or cooking methods of the red meats included in individual studies.
consistent as for processed meats. The authors noted that some of this may be due to differences in saturated fat content or cooking methods of the red meats included in individual studies.
But this analysis also showed that the effect of red meat on heart disease risk may be dose dependent. For example:
-
- The studies they reviewed suggested that consuming ≥2 servings per day of red meat is associated with a 27% increased risk of heart disease. However, consuming <3 servings per week may not increase risk.
-
- The idea that the effect of red meat on heart disease risk may be dose-dependent is novel. However, the authors said we also need to ask what replaces red meat in the diet. They postulated that when red meat consumption is decreased, it is often replaced with healthier protein sources.
- White meat such as poultry does not appear to affect heart disease risk. This has been predicted by earlier reports, but this analysis strengthens those predictions.
- Fish consumption decreases heart disease risk. This is not new. But this review added precision about recommended fish intake (2-4 servings/week) and a couple of caveats:
-
- The heart benefits of fish may be due to their omega-3 content and may not apply equally to fish with lower omega-3 content.
-
- The authors also expressed concerns about the sustainability of high-omega-3 fish populations. I would also add that our oceans are increasingly polluted, so contamination is another concern.
- Egg consumption up to one egg/day does not appear to increase heart disease risk. This is consistent with the
 current American Heart Association recommendations.
current American Heart Association recommendations.
However, the authors noted that the effect of eggs on serum cholesterol, and hence heart disease risk depends on several factors.
-
- Genetics, obesity, and diabetes can make it more difficult to regulate serum cholesterol levels. For these individuals, eggs may need to be eaten only sparingly.
-
- Diets low in saturated fat and high in fiber from plant foods help the body regulate serum cholesterol. Several studies suggest that eggs may decrease heart disease risk in the context of this type of diet.
- Dairy: Neither low-fat nor high-fat dairy foods appear to influence heart disease risk. This is different from the standard recommendation to consume low-fat dairy foods. But it is in line with the trend of recent research studies on dairy and heart disease.
Once again, there were a couple of caveats:
-
- There is increasing evidence that fermented dairy foods may decrease heart disease risk which may explain why certain high-fat cheeses and other high-fat fermented dairy foods appear to have a neutral or slightly beneficial effect on heart disease risk.
-
- As with eggs the effect of high-fat dairy foods on heart disease risk may be influenced by genetics and diet context.
Foods Of Plant Origin: The effect of plant foods have been known for some time, and the most recent studies included in this analysis have not changed those conclusions.
- Fruits and Vegetables consistently reduce heart disease risk in multiple studies. In each case, the optimal
 intake appears to be about 2 servings of each per day which provides an 18-21% risk reduction for vegetables and a 21-32% risk reduction for fruits.
intake appears to be about 2 servings of each per day which provides an 18-21% risk reduction for vegetables and a 21-32% risk reduction for fruits.
- Legumes (beans and peas) also consistently reduce heart disease risk in multiple studies. At the optimal intake of around 4 servings per week the risk reduction is around 14%.
- Nuts also consistently reduce heart disease risk. At the optimal intake of around one serving (a handful) per day, the risk reduction is around 25%.
- Cereals (grains) were divided into 3 categories:
-
- Refined carbohydrates with a high glycemic index (e.g., white rice, white bread) are associated with increased heart disease risk in multiple studies probably due to their effect on blood sugar levels. And the increased risk is significant (Around 66% higher risk for every 2 servings).
-
- Refined carbohydrates with a low glycemic index (e.g., pasta, corn tortillas) show an inconsistent effect on heart disease risk.
-
- Whole grains are consistently associated with a lower heart disease risk. Two servings of whole grains per day are associated with a 25%-34% decreased risk.
Miscellaneous Foods:
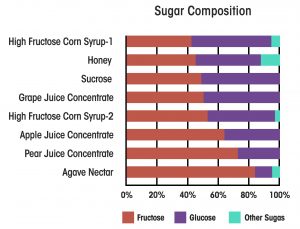
- Soft Drinks are associated with increased heart disease risk. One serving per day increases the risk by around 15-22% and recent evidence suggests that artificially sweetened soft drinks offer no heart health benefits compared to sugar sweetened soft drinks.
- Coffee and Tea are both associated with decreased heart disease risk. For coffee the optimal benefit may occur at around 3 cups/day. Higher levels may have an adverse effect on heart disease risk.
Summary of Heart Health Recommendations
 If you are thinking that was a lot of information, the authors provided a numerical summary of their recommendations for a heart-healthy diet. They are:
If you are thinking that was a lot of information, the authors provided a numerical summary of their recommendations for a heart-healthy diet. They are:
- Two servings per day of vegetables, fresh fruits, and whole grains.
- One serving per day of nuts and seeds, low-glycemic index refined cereals, extra-virgin olive oil or non-tropical vegetable oils, and yogurt.
- Four servings per week of legumes and fish.
- No more than 3 servings per week of white meat, eggs, cheese, and milk.
- No more than 2 servings per week of high-glycemic index refined starchy foods, red meat, and butter.
- Only occasional consumption of processed meats.
What Does This Study Mean For You?
 Of course, nobody wants to follow a “diet by the numbers”. If you are like most of us, you want flexibility and you want to be able to eat some of your favorite foods. So, let me put these recommendations into a more “user friendly” form.
Of course, nobody wants to follow a “diet by the numbers”. If you are like most of us, you want flexibility and you want to be able to eat some of your favorite foods. So, let me put these recommendations into a more “user friendly” form.
If you want a healthy heart:
- Whole, unprocessed or minimally processed, plant foods are your friends.
- Your heart-healthy foundation should be fruits, vegetables, whole grains, nuts and seeds, healthy plant oils, and legumes.
- Your heart-healthy foundation can also include fermented dairy foods and low-glycemic index refined grains.
- Your “go-to” beverages should be water, tea (both caffeinated and herbal teas), and coffee. You should avoid soft drinks and other sugar-sweetened or artificially sweetened beverages.
- Once you have achieved a heart-healthy foundation you can add a few servings per week of white meat, eggs, cheese, and dairy, even high-fat dairy.
- If you have good adherence to the heart-healthy foundation described above and no genetic or health issues that increase your risk of heart disease, you can probably eat more of these foods.
- Conversely, if your adherence to the heart-healthy foundation is poor and/or you are at high risk of heart disease, you may wish to consume less of these foods.
- If you have good adherence to the heart-healthy foundation, you can also add up to 1-2 servings of high-glycemic index refined carbohydrates, red meat, or butter per week. With red meat, you may want to consider it as a garnish that adds flavor to a plant-based meal rather than the centerpiece of the meal.
- You should eat processed meats seldom or never.
The Bottom Line
A new comprehensive review and meta-analysis of 99 clinical studies with tens of thousands of participants has updated the correlation between foods and heart disease risk.
Many of the recommendations based on this analysis are identical to previous recommendations for a heart-healthy diet.
But there are some subtle changes to those recommendations based on the latest data.
For more details about this study and what a heart-healthy diet might look like for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.