How Does This Relate To Pregnancy, Labor, Birth, And The Postpartum Period?
Author: Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN
Editor: Dr. Steve Chaney
Family History And Pregnancy
 On the first prenatal appointment, an extensive history is taken that includes family history, personal medical history, gynecological history, pregnancy history; sexual history, social history.
On the first prenatal appointment, an extensive history is taken that includes family history, personal medical history, gynecological history, pregnancy history; sexual history, social history.
Due to the many physiological changes that occur during pregnancy, birth and the postpartum period, one can be placed at increased risk for the development of health conditions that may not have been present prior to pregnancy.
A properly collected and granular family history may determine if a woman is at increased risk for disease, identify early warning signs of disease; and assist the provider in recommending treatments for reducing a woman’s risk for developing serious problems in during pregnancy, labor, birth and the postpartum period.
A recent study (D Rasooly et al, J Am Heart Assoc, 12(22): e030779, 2023) published in 2023 presents findings on the association between a comprehensive family history that includes parents, siblings and the self-reported personal history of obesity, diabetes, and heart and blood conditions.
How Was This Study Done?
The study involved 125,430 participants; 66.3% were women; 33.75 were men; 75.7% were White; 10.4% were Hispanic; 3.3% were Asian; 8.3% were Black and 2.4% were Other.
The study provided information on the possibility of someone developing a health problem based upon their family history. It also reported odds ratio (statistical probability) of other conditions developing when one health condition was present.
The Importance Of Family History For Maternal Health
 The findings of the study were as follows. Of the 125,430 participants:
The findings of the study were as follows. Of the 125,430 participants:
- A family history of hypertension or high blood pressure was reported by 51.6% of the participants. When this was disaggregated by race, 60% of Blacks reported having a family history of hypertension and 54.4% of Asians reported having hypertension compared to 48.6% of Whites.
- A family history of high cholesterol was reported by 38.7% of the participants.
- A family history of heart attack was reported by 23.6% of the participants.
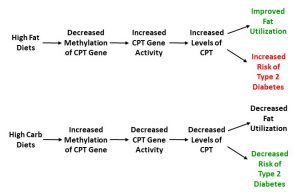
- A family history of Type 2 diabetes was reported by 21.4% of the participants.
If one has a family history of a certain medical condition, there is an increased likelihood that this same condition can be passed on to the next generation (in this case, the pregnant mother). The statistical term “odds ratio” means the likelihood of this same condition occurring in the next generation when there is a family history vs when there is not a family history.
Passing the Same Disease Down To The Pregnant Mother
Compared to those who do not have a family history, here are the odds for passing down these same conditions to the mother.
- Hypertension – 2.56 times the odds it can be passed down.
- High cholesterol – 2.89 times the odds. If there is a family history of high cholesterol, there is 2.44 odds of Asians developing high cholesterol compared to 2.16 odds in the Black population.
- Coronary Artery Disease – 3.54 the odds.
- Type 2 diabetes – 3.79 times the odds.
- Anemia – 2.66 times the odds.
- Peripheral vascular disease – 6.60 times the odds.
- Pulmonary embolism/deep vein thrombosis – 5.60 times the odds.
- Obesity – 1.2 times the odds. If there is a family history of obesity, for Asian populations, there is 2.93 odds that obesity will be passed down to son or daughter. This ratio is 4.57 in the Black population.
Passing Another Disease Down To The Pregnant Mother
The study also reported the association of family history to someone’s personal health condition and the odds of the pregnant mother developing a different health condition pertaining to obesity, diabetes and heart and blood. On average there was 1.5 odds of developing a different condition from the condition reported in the family history. For example:
- When there is a family history of Type 2 diabetes, there is 2.04 odds of developing obesity.
- When there is a family history of pulmonary embolism/deep vein thrombosis; there is 3.25 odds of developing a bleeding disorder.
 The two family health conditions that had the most evidence of association with other conditions were family history of stroke and heart attack.
The two family health conditions that had the most evidence of association with other conditions were family history of stroke and heart attack.
When there is a family history of stroke, the odds of the pregnant mother developing other conditions are as follows:
- Obesity (1.35).
- Heart attack (1.7). There was almost double the odds ratio in the Hispanic population with 3.34 odds.
- Hypertension (1.40). Whites reported 1.37 odds for developing hypertension compared to 1.55 for Blacks and 1.43 for underrepresented populations.
- High cholesterol (1.33). When disaggregated by race, Whites had a 1.29 odds ratio; Black a 1.60 odds ratio and those underrepresented in biomedical research had a 1.33 odds ratio.
When there is a family history of heart attack, the odds of the pregnant mother developing related conditions are as follows:
- Heart attack (2.17). These odds are decreased for Asians (1.92) and Hispanics (1.27).
- Coronary artery disease (1.97).
- Congestive heart failure (1.54).
- High cholesterol (1.44).
When there is a family history of Type 2 diabetes, the odds of the pregnant mother developing other conditions are:
- Heart attack (1.32).
- Congestive heart failure (1.44).
- Bleeding disorder (1.26).
- Coronary artery disease (1.37 odds).
- Asians with a family history of Type 2 diabetes have a 1.79 odds of developing heart valve disease.
How Does This Relate To Pregnancy, Labor, Birth, And The Postpartum Period?
 The five main causes for pregnancy related death in the United States (defined as maternal death up until 12 months after giving birth) are:
The five main causes for pregnancy related death in the United States (defined as maternal death up until 12 months after giving birth) are:
- Mental Health – 24%.
- Hemorrhage – 14%.
- Cardiovascular Disease – 13%.
- Cardiomegaly (enlarged heart) – 9%.
- Blood Clots – 9%
Many of these causes are related to the cardiovascular system. Based upon the data in this study, a family history of any of the following can contribute to the increased odds of developing health problems during pregnancy:
- Stroke
- Type 2 diabetes
- Pulmonary embolism/deep vein thrombosis
- Hypertension
- Anemia
Once someone knows their family history, when planning for a pregnancy, they can work on any nutrition or lifestyle changes needed to reduce the incidence of problematic health conditions occurring during pregnancy and the health of the newborn.
The US Surgeon General has published My Family Health Portrait which will allow individuals to record and share their family history. It can be accessed at https://cbiit.github.io/FHH/html/index.html
The Bottom Line
- When planning a pregnancy, a thorough family health and personal history is important.
- Obesity, diabetes and heart and blood conditions can be passed from parents to children. Some of these conditions include anemia, peripheral vascular disease, pulmonary embolism/deep vein thrombosis, Type 2 diabetes, hypertension, coronary artery disease, and high cholesterol.
- There is an association between a family history of stroke and heart attack and numerous other health conditions.
- One’s family history can impact health conditions experienced during pregnancy that can result in pregnancy-related death up to 12 months after the baby is born.
- The US Surgeon General’s My Family Health Portrait is an online tool that can help families to record their family health history and share with other family members.
For More Information
Feel free to visit my website, subscribe to my YouTube channel and learn more about my online coaching program, “Mastering Pregnancy and Birth”.
You-Tube Channel (https://www.youtube.com/channel/UCPMch7GamgUYYd9H3GonJZQ) – Over 80 videos exploring pregnancy, labor, birth, postpartum and contraception
www.thecarabcompany.com (https://www.thecarabcompany.com/) – Website with free downloadable pregnancy and birth information
Mastering Pregnancy and Birth Coaching Program (https://www.thecarabcompany.com/healthy-pregnancy-to-healthy-birth-accelerator) – A program that prepares Dads and Mom’s-to-be for a healthier pregnancy and safer birth. This course also provides information for Doulas to provide enhanced support to families.
Carolyn Curtis
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.
_____________________________________________________________________________
The posts on this website and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
______________________________________________________________________
About The Author
 Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN, has:
Carolyn Curtis, MSN, CNM, RN, FACNM, FAAN, has:
More than 40 years’ experience in the oversight of domestic and international programs and the provision of nursing and midwifery integrated service delivery in maternal child health, family planning, reproductive and women’s health care.
Twenty years’ experience in teaching, mentoring, and providing clinical oversight to undergraduate and graduate public health, medical, nursing and midwifery students.
About The Editor
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.