What About Primarily Meat-Based Diets?
Author: Dr. Stephen Chaney

It’s so confusing. Everyone claims they have clinical proof that their diet is the best. You will be healthier and live longer.
But the diets are so different. They range from vegan to keto. They can’t all be equally healthy. What is the truth?
To answer that question, we first need to understand how the proponents of each diet can claim theirs is the perfect diet for health and longevity. It’s because they base their claims on:
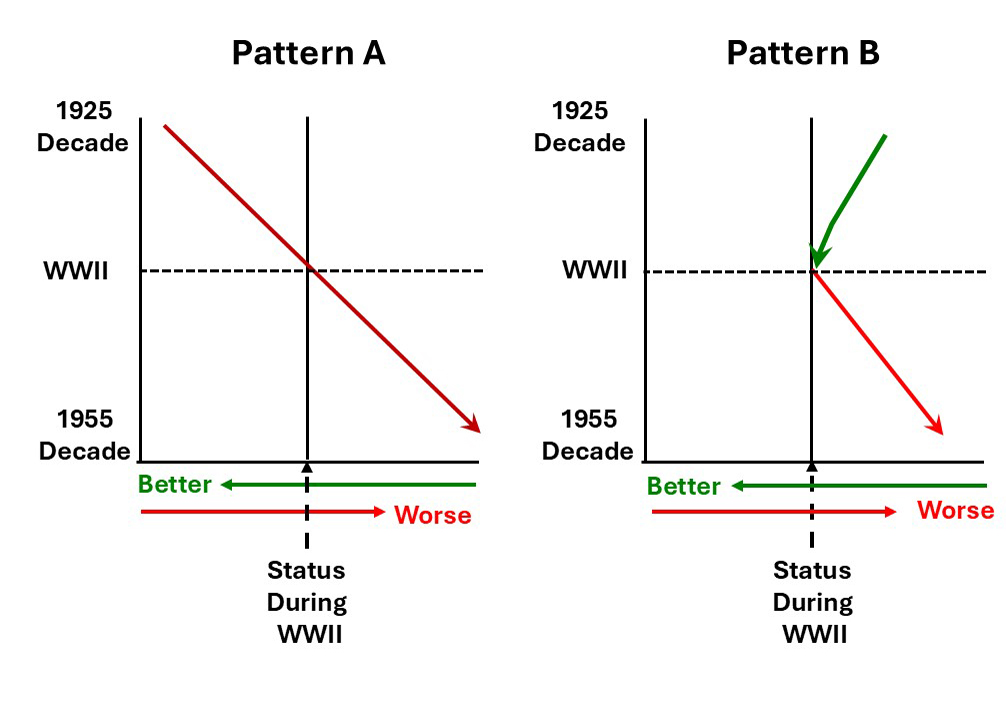
- Short-term studies. Most of their claims are based on studies that range from a few weeks to a few months. You need 20- or 30-year studies to measure the effects of a particular diet on health outcomes.
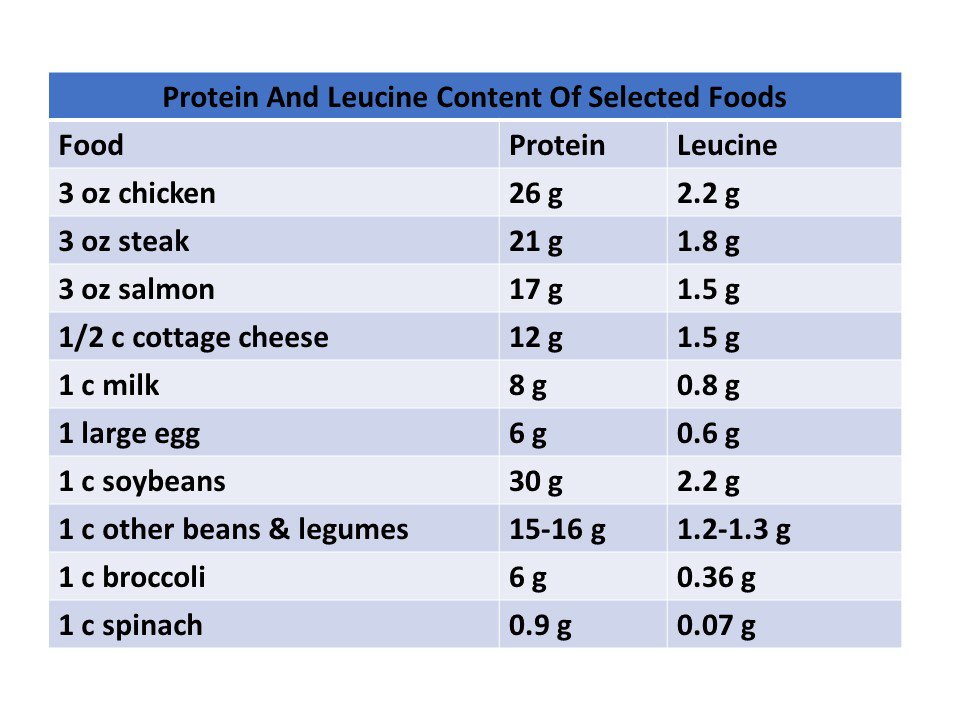
- Biological markers (Things like cholesterol and triglyceride levels, blood sugar control, and/or inflammation). Biological markers can predict possible health outcomes. But without long-term studies on actual health outcomes, you don’t know whether those predictions are accurate.
- Comparisons with the typical American diet. Any diet looks good compared with the American diet.
- Elimination of highly processed foods. While these diets emphasize different foods, they are all whole food diets. Again, any diet that eliminates processed foods is an improvement.
-
- It doesn’t matter whether you restrict calories, restrict certain foods or food groups, or restrict the time you allow yourself to eat. You unconsciously eat less.
-
- And when you eat less, you lose weight.
-
- And when you lose weight, your cholesterol and triglyceride levels fall, your blood sugar control improves, and inflammation decreases.
-
- That’s why short-term weight loss and improvement in biological markers are virtually identical with vegan and keto diets. Those diets are as different as any two diets could be. But they are both highly restrictive diets.
The take-home lesson is clear. Don’t be confused by claims based on short-term studies. What you should look for is:
- Long-term studies (20 years or more)…
- that look at the effect of diet on health outcomes, and…
- do not compare their diet with the typical American diet.
When I first reviewed this topic 8 years ago, I could only find a few studies that met these criteria:
- One study showed that people consuming primarily plant-based diets weighed less than people who consumed primarily meat-based diets for 20 years or more.
- Other studies showed that people consuming primarily plant-based diets had a reduced risk of diabetes and heart disease compared to people consuming primarily meat-based diets for 20 years or more.
These are valuable observations, but they are limited. That’s why I was so excited when I came across a recent 30-year study (A-J Tessier et al, Nature Medicine, volume 31, pages 1644-1652, 2025) looking at the effect of 9 different diets on longevity and health outcomes. In short, this study looked at the effect of different diets on healthy aging.
How Was This Study Done?
 The authors of this study used data from 105,015 participants in the Nurses’ Health Study (NHS) and Health Professionals Follow Up Study (HPFS). Both studies enrolled participants in 1986 and followed them through 2016. In short, they were both 30-year studies. Participants with preexisting chronic diseases were excluded from the study.
The authors of this study used data from 105,015 participants in the Nurses’ Health Study (NHS) and Health Professionals Follow Up Study (HPFS). Both studies enrolled participants in 1986 and followed them through 2016. In short, they were both 30-year studies. Participants with preexisting chronic diseases were excluded from the study.
- Lifestyle factors and medical histories were assessed every two years.
- A detailed dietary assessment was conducted every four years. The assessments measured the intake of 152 foods. Food intakes were averaged over the duration of the study for each participant.
[Note: This study did not measure how the diets of participants changed between 1986 and 2016, although that is an interesting question. Perhaps a future study is planned.]
Based on the foods eaten, the diets of the participants were evaluated for adherence to 9 dietary patterns, which I have described in more detail below.
[Note: To be clear, the participants were not trying to follow these diets. They ate what they ate, and the investigators subsequently compared their dietary pattern with various healthy diets.]
For each of the diets included in this study, participants were divided into quintiles based on how closely their food intake adhered to the recommendations for that diet. Then the highest quintile was compared to the lowest quintile to determine how well that diet predicted “healthy aging” after a 30-year follow-up.
The term “healthy aging” was based on 5 criteria:
- Longevity – achieving an age of 70 or more.
- Absence of the top 11 major chronic diseases (cancer, diabetes, myocardial infarction (heart attack), coronary artery disease, congestive heart failure, stroke, Parkinson’s disease, multiple sclerosis, and ALS).
- No impairment of cognitive function.
- No impairment of physical health.
- No mental health issues.
In other words, these were not just individuals who survived 70 years or more. They survived and thrived. They were enjoying their golden years because they still had good health and excellent quality of life.
Diets Included In This Study
 The diets included in this study were:
The diets included in this study were:
- AHEI – Alternative Healthy Eating Index (A scoring system developed by Harvard researchers to measure overall diet quality based on its ability to predict lower risks of heart attacks, strokes, and diabetes).
- aMed – Alternative Mediterranean Diet Index (The aMed diet index differs from the original Med index by separating fruits and nuts into different groups, eliminating dairy, emphasizing whole grains, and excluding red and processed meats in favor of chicken and fish).
- DASH – Dietary Approaches to Stop Hypertension (The name speaks for itself. But I also sometimes refer to this diet as “the Americanized version of the Mediterranean diet’ because it features foods more familiar to Americans. For example, it allows more red meat options than most of the other diets in this list.
- MIND – Mediterranean-Dash intervention for Neurogenerative Delay (It is a dietary pattern designed to reduce the risk of Alzheimer’s disease and other forms of dementia. It combines elements of the Mediterranean and DASH diets but differs from both by emphasizing berries as a major fruit source, among other things.)
- hPDI – Healthy Plant-Based Diet Index (It is a scoring system that measures adherence to a diet rich in healthy plant-based foods and lower consumption of less-healthy plant foods and animal foods.)
- PHDI – Planetary Health Diet Index (It emphasizes foods (primarily plant foods) that are healthy and are good for the environment. Of the diets on this list, it is the most restrictive and closest to a vegan diet)
- EDIH – Empirical Dietary Index For Hyperinsulinemia (It is a scoring system that measures the potential of a diet to cause chronically high insulin levels, which is associated with type 2 diabetes and certain cancers.)
- EDIP – Empirical Dietary Inflammation Pattern (It is a scoring system that measures the inflammatory potential of a diet.)
- UPF – Consumption of Ultraprocessed Foods (Since recent studies have shown that most Americans get between 55 and 70% of their calories from ultraprocessed foods, this is fast becoming a measure of the typical American diet.)
Note: Except for the UPF diet, these are all whole food, primarily plant-based diets.
What Diet Is Best For Healthy Aging?
 Here are the results of the study (drum roll, please):
Here are the results of the study (drum roll, please):
- Of the 105,015 participants in this study, only 9.3% achieved healthy aging.
- Adherence to any of the 8 healthy diets improved the probability of achieving healthy aging.
- The odds of achieving healthy aging ranged from 1.45 for the Healthy Plant-Based Diet to 1.86 for the Alternative Healthy Eating Index.
- If you were to pick one winner, it would be the Alternative Healthy Eating Index. And if you were to define healthy aging as achieving an age of 75 or more with the other 4 criteria, the odds increase to 2.24 (more than double) for the Alternative Healthy Eating Index.
- As you might expect, adherence to a diet high in ultraprocessed foods had the opposite effect. It decreased the odds of achieving healthy aging by 32%.
When you look at each of the criteria for healthy aging individually, the results were a bit more nuanced:
- For survival to 70+ years, the Alternative Healthy Eating Index and the Planetary Health Diet Index were tied. Both increased the odds of survival by more than 2-fold.
- The Alternative Healthy Eating Index and the Planetary Health Diet Index were also tied for surviving to 70 with intake cognitive health and intact physical function.
- The Empirical Dietary Index For Hyperinsulinemia edged out the Alternative Healthy Eating Index for freedom from 11 chronic diseases.
The effect of healthy diets on the odds of achieving healthy aging is independent from BMI, smoking, and physical activity. This means that:
- The effects of healthy diets on healthy aging were not because people consuming healthy diets weighed less, smoked less, or exercised more.
- Even if some of your lifestyle choices are suboptimal, choosing a healthy diet will increase your odds of surviving and thriving.
Finally, the study looked at the effects of individual foods on healthy aging. The results were:
- Higher intakes of fruits, vegetables, whole grains, unsaturated fats, nuts, legumes, and low-fat dairy products increase your odds of healthy aging.
- Higher intakes of trans fats, sodium, sugary beverages, and red or processed meats decrease your odds of achieving healthy aging.
The effects of these foods on healthy aging aren’t novel. They are consistent with dozens of other studies that have looked at the effect of individual foods on long-term health outcomes. In fact, the diets included in this study were chosen because they included foods that positively affect health outcomes and minimize foods that negatively affect health outcomes.
What About Primarily Meat-Based Diets?
 I have good friends who advocate for primarily meat-based diets such as keto, paleo, and carnivore. I’m sure they are going to say, “This study is a sham. It only included primarily plant-based diets, so, of course, it is only going to show benefits for primarily plant-based diets.” I can hear their their questions now:
I have good friends who advocate for primarily meat-based diets such as keto, paleo, and carnivore. I’m sure they are going to say, “This study is a sham. It only included primarily plant-based diets, so, of course, it is only going to show benefits for primarily plant-based diets.” I can hear their their questions now:
- Why didn’t this study include any of the primarily meat-based diets? My answer is: “All the popular meat-based diets exclude one or more of the food groups associated with health and longevity and emphasize one or more of the food groups associated with a shorter, less healthy life. And these food associations are consistent among multiple long-term studies looking at the effect of various foods on health outcomes.
The authors could have constructed a similar index for each of the popular meat-based diets. But they would have been the inverse of the plant-based diet indices because the foods included and excluded from plant-based and meat-based diets are opposite. Therefore, just like the UPF index, they would have been associated with a decreased probability of achieving healthy aging.”
- Why did the scientists designing this study ignore the proven health benefits of primarily meat-based diets? My answer is: “The “proven benefits” of primarily meat-based diets are based on short-term studies showing the effects of those diets on biological markers. Long-term studies looking at health outcomes are lacking.”
- But modern primarily meat-based diets are a special case because they limit carbohydrates and cause ketosis. Why weren’t they included in the study? My answer is: “The Atkins diet limits carbohydrates and causes ketosis. It has been around for more than 50 years. And, to my knowledge, there are no studies showing it is beneficial long term. If the Atkins diet cannot be shown to have long-term health benefits, it is unlikely that modern diets that mimic it are healthy long term.
What Does This Study Mean For You?
 The answer is clear. If you want to survive and thrive in your 70s and beyond, choose a whole food, primarily plant-based diet.
The answer is clear. If you want to survive and thrive in your 70s and beyond, choose a whole food, primarily plant-based diet.
If you want the absolute best diet, follow the Alternative Healthy Eating Index recommendations. There are many online resources to guide you.
However, any whole food, primarily plant-based diet will do. The ones with the most online resources are the Mediterranean, DASH, and MIND diets. Choose the one that best fits your food preferences and lifestyle.
If you want to go more vegetarian, the Healthy Plant-Based Diet is a bit easier than a strict vegan diet.
If you are concerned about the environment, the Planetary Diet is best for you.
If you have specific health issues like hypertension, diabetes, or inflammation, there are diets designed just for you.
And if following structured diets is not your style, just:
- Eat more fruits, vegetables, whole grains, unsaturated fats, nuts, legumes, and low-fat dairy products.
- Eat less trans fats, sodium, sugary beverages, and red or processed meats, and ultraprocessed foods.
Finally, even if some of your lifestyle choices are suboptimal, this study shows choosing a healthy diet will increase your odds of surviving to your 70s and thriving.
The Bottom Line
A recent 30-year study looked at the effect of 8 whole food, primarily plant-based diets on healthy aging defined as:
- Achieving an age of 70 or more.
- The absence of the top 11 major chronic diseases.
- No impairment of cognitive function.
- No impairment of physical health.
- No mental health issues.
The key findings were:
- Adherence to any of 8 whole food, primarily plant-based diets improved the probability of achieving healthy aging.
- The odds of achieving healthy aging ranged from 1.45 for the Healthy Plant-Based Diet to 1.86 for the Alternative Healthy Eating Index.
For more information on this study, why primarily meat-based diets were not considered healthy enough to be included in this study, and what this study means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading Biochemistry textbooks for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.