Don’t Fall For Misleading Marketing Claims
Author: Dr. Stephen Chaney
 There are lots of multivitamin-multimineral products in the marketplace. Every company must differentiate their product from the competition to win their market share. When that differentiation is based on quality, purity, and clinical proof the product works, I am all for it. May the best company win.
There are lots of multivitamin-multimineral products in the marketplace. Every company must differentiate their product from the competition to win their market share. When that differentiation is based on quality, purity, and clinical proof the product works, I am all for it. May the best company win.
However, the pressure to win market share is intense. Quality controls and clinical studies are expensive. All too often companies try to differentiate their multivitamin-multimineral products based on marketing hype and/or worthless ingredients that subtract money from your wallet without adding anything of value to your health.
With so many claims and counter claims in the marketplace, it has become almost impossible for the average consumer to know which claims are true and which are false. Everyone wants to get the best multivitamin-multimineral for their health at the least possible cost. Perhaps that is why I am so frequently asked for guidance on how to choose the best multivitamin.
In this week’s article, I will give you 6 tips you can use to select the multivitamin-multimineral product that is best for you. I will tell you what to look for in a good multivitamin and which marketing claims you should just ignore.
But first, we need to look at how nutritional standards are set.
How Are Nutritional Standards Set?
 The standards for nutritional supplements are set in a two-step process.
The standards for nutritional supplements are set in a two-step process.
Step 1: In the first step, The Institute of Medicine (IOM) of the National Academies of Sciences selects a committee of experts called the Food and Nutrition Board to set standards for a specific set of nutrients. They set 3 kinds of standards:
- Recommended Dietary Allowances or RDAs are the average daily dietary intake level sufficient to meet the nutrient requirements of nearly all (97-98 percent) healthy individuals in a group.
- Adequate Intakes or AIs are established when evidence is insufficient to develop an RDA and are set at a level assumed to ensure nutritional adequacy.
- Where toxicity is a potential concern, Tolerable Upper Limits or ULs represent the maximum daily intake unlikely to cause adverse health effects.
- Just to confuse things, all three standards are part of what is called Dietary Reference Intakes or DRIs.
Step 2: The DRIs are specific for age, gender, pregnancy & lactation. It would be hopelessly complicated to use DRIs for nutrition labels on foods and supplements. Therefore, the FDA sets a Daily Value (DV) for the purposes of food and supplement labeling. Originally, DVs were set based on the highest DRI for a specific nutrient. However, currently the DV is an average of DRIs for adults and children 4 years and older. It is not identical to the RDA or DRI for any specific group, but it is a useful standard for supplement labels.
With this information in mind, let’s get back to the 6 tips for choosing the best multivitamin.
#1: Good Product Design Matters
 Comparing nutrition labels on multivitamin-multimineral supplements can be tricky. Some supplements only provide 5-10% of the Daily Value (DV) for some nutrients. Are those nutrients unimportant? Some supplements provide hundreds or thousands % of the DV for other nutrients. Is more better?
Comparing nutrition labels on multivitamin-multimineral supplements can be tricky. Some supplements only provide 5-10% of the Daily Value (DV) for some nutrients. Are those nutrients unimportant? Some supplements provide hundreds or thousands % of the DV for other nutrients. Is more better?
Often companies will quote some random scientist or one or two clinical studies to support the mix of nutrients they include in their multivitamin-multimineral supplement. Don’t fall for their marketing hype.
The only valid nutritional standards for multivitamin-multimineral products in the United States are the DV standards set by the Food & Nutrition Board of the Institute of Medicine. They are the standards you should look for in evaluating nutrition labels.
That’s because the National Academies of Sciences is the real deal. The National Academies represents the top 1-2% of scientists in the country. To be selected to the National Academies you must be nominated by an Academy member and voted on by the entire Academy. Selection is based on your research contributions over decades. (No, I am not a member of the Academy, but thanks for thinking that question).
The Institute of Medicine of the National Academies of Sciences selects the best of the best to serve on the Food and Nutrition Board. They are world renowned experts who review all the pertinent literature (not just one or two studies) They decide on which nutrients are essential and how much of them we need.
It always amazes me that some companies pretend they know more than the Food and Nutrition Board. It amazes me even more that some people believe those companies.
With that in mind, this is what to look for when comparing nutrition labels:
- The FDA has set Daily Value (DV) recommendations for 24 vitamins and minerals (23 if the supplement is for adult men or postmenopausal women and does not contain iron). Make sure your multivitamin-multimineral has all 24. Count them. If a company leaves out an essential nutrient, they are not required to list it on the label.
- The Food and Nutrition Board has classified several other nutrients as essential but does not feel there have been enough studies to establish a DRI. Without a DRI, the FDA cannot set a DV. Those nutrients are represented with a “dagger” symbol on the label with the footnote “Daily Value not established”. These can be useful additions to a multivitamin-multimineral supplement, provided they are not present in excess.
- Ignore anything companies list on their nutrition labels that does not have a %DV value or a “dagger” symbol. This is often just marketing hype. In some cases, the ingredients have no proven benefit. In many other cases, it’s just not possible to put enough of them in a multivitamin-multimineral tablet to provide any real benefit.
#2: Look For Balance
 This is another area in which we need to be guided by the recommendations of the Food and Nutrition Board of the Institute of Medicine. One of the reasons many experts recommend that people get their vitamins and minerals from foods rather than from supplements is because many supplements are unbalanced. That’s a problem because there are many cases in which too much of one nutrient can interfere with the absorption or metabolism of related nutrients. For example,
This is another area in which we need to be guided by the recommendations of the Food and Nutrition Board of the Institute of Medicine. One of the reasons many experts recommend that people get their vitamins and minerals from foods rather than from supplements is because many supplements are unbalanced. That’s a problem because there are many cases in which too much of one nutrient can interfere with the absorption or metabolism of related nutrients. For example,
- Zinc and copper compete for absorption. For best absorption and maximal utilization by the body, the zinc to copper ratio should be close to 1:1 based on DV.
- B vitamins should be in balance. Look for a multivitamin-multimineral supplement that provides 100-200% of the DV for all 8 essential B vitamins. (The levels can be higher in a B Complex supplement, but they should still be in balance.)
Some manufacturers will leave out the expensive B vitamins and load up on the cheap ones. This saves them money. It also allows them to use marketing terms like “mega” or “super”. A supplement that provides 50% or less of the DV for some B vitamins and 1,000% or more of the DV for others is ridiculous. There is absolutely no rationale for a ratio like that except to mislead consumers.
- As for the other nutrients in multivitamin-multimineral supplements, they should not be significantly below 50% or significantly above 250% of the DV.
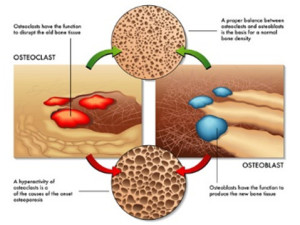
- Calcium, magnesium, and phosphorous are a special case. They are bulky, so many manufacturers only provide 5-10% of them in their multivitamin-multimineral supplements. This is not ideal because many of the nutrients in a multivitamin-multimineral supplement are required for optimal utilization of calcium and magnesium in bone formation.
Many Americans get only 50% of the DV for calcium and magnesium in their diet. Thus, it makes good sense to provide 30-50% of the DV for calcium and magnesium in a multivitamin multimineral supplement. Most Americans get close to the DV for phosphorous from their diet, so the amount of phosphorous in a supplement is not particularly important.
#3: Don’t Fall For The Hype
 In their attempts to differentiate themselves, many companies claim that they use a more natural or a better utilized form of the vitamin or mineral than their competitors. Ignore those claims. They are just marketing hype. For example,
In their attempts to differentiate themselves, many companies claim that they use a more natural or a better utilized form of the vitamin or mineral than their competitors. Ignore those claims. They are just marketing hype. For example,
- In previous issues of “Health Tips From the Professor” I have debunked the claims that folate and methyl folate are more natural, safer and more effective than folic acid. The claims that alternate chemical forms of other vitamins are more natural, safer, and more effective are equally bogus.
- The claims by some manufacturers that they use a form of calcium that is more readily absorbed are not just misleading. That is the wrong question. Calcium in our bloodstream can do bad things (like calcification and hardening of the arteries) if it is not quickly utilized for bone formation.
-
- Thus, the important question is how well the calcium is utilized for bone formation. Look for clinical studies showing that the calcium in their multivitamin-multimineral supplement is efficiently utilized for bone formation rather than hype about how quickly it gets into the bloodstream.
- There is a good reason that many supplement companies continue to use ingredients like folic acid for B9, cyanocobalamin for B12, pyridoxine for B6, etc. All of them are supported by hundreds of clinical studies showing that they are safe and effective. I have no issue with companies choosing to use different forms of these vitamins. Just don’t fall for their hype that the forms they are using are somehow more natural, safer or more effective than the traditionally used forms of the same vitamin.
#4: Don’t Fall For Buzz Words

Some manufacturers attempt to differentiate their products by claiming they are natural, organic, non-GMO, or are made from food. The companies are attaching buzz words to their product that they know resonate with the American people. Don’t believe them. Those claims are all bogus. They are marketing hype. For example,
- There is no standard for “natural” so companies are not required to provide any evidence to back up their claim. If they claim that their product is natural, ask for a detailed list of the source and processing method for all their ingredients. If they are unwilling or unable to provide you with that information, don’t believe their claim of natural.
- “Organic” certification for a supplement simply means that ingredients come from crops raised using organic methods. It is no guarantee of purity. Organically grown crops can still be contaminated if the air, soil or water is contaminated from any nearby pollution source. For example, ground water pollution is the major source of heavy metal contamination often seen in rice-derived ingredients. It is far more important to select your supplement based on rigorous quality control standards that assure it is pure than to rely on “organic” on the label.
- A “non-GMO” designation is useful for foods and for protein, but it is meaningless for the ingredients in a multivitamin-multimineral supplement. Those ingredients have been extensively purified. They contain no genetic information. They are chemically indistinguishable from purified ingredients obtained from GMO sources. If you would like more detailed information about the GMO controversy, I have provided a balanced perspective on GMO in a video.
- Claims by some companies that their vitamins are derived from foods are completely bogus. That is a physical impossibility. For example, let’s look at what it would take to provide the DV for just 3 of the nutrients in a single multivitamin pill, assuming they started with the best food sources of those 3 nutrients:
-
- It would take 1 cup of cooked lentils, 2 cups of cooked spinach, or 4 cups of cooked broccoli to provide the DV for folic acid.
-
- It would take 1 cup of sunflower seeds, 1.5 cups of pistachio nuts, or 7 ounces of cooked tuna to provide the DV for vitamin B6.
-
- It would take 5 ounces of cooked chicken breast, 1 cup of peanuts, or 6 cups of green peas to provide the DV for niacin.
That’s just 3 nutrients and one multivitamin tablet. You do the math. If they lie to you about their vitamins coming from food, they will probably lie about other things as well.
#5: Don’t Fall For Scare Tactics
 Some companies try to scare you into buying their products by claiming their competitors are using unsafe ingredients. These claims are usually bogus, but it is useful to understand where this misinformation comes from.
Some companies try to scare you into buying their products by claiming their competitors are using unsafe ingredients. These claims are usually bogus, but it is useful to understand where this misinformation comes from.
There is a lot of unfounded hysteria on the internet about product ingredients. Much of this hysteria has been fueled by a few well-known bloggers. I believe their intentions were pure in the beginning. They started by warning the public about truly dangerous ingredients like artificial colors, flavors, preservatives and sweeteners.
However, blogging has a dark side. To capture a large audience, your blog posts need to be sensational every week. As the weeks go by it becomes harder and harder to find subject matter that is both sensational and accurate. That’s when some bloggers go over to “the dark side”.
They become more concerned about the size of their audience than the accuracy of the information they post. They start vilifying ingredients that are perfectly safe as long as the manufacturer purifies them correctly and tests them for purity. These are ingredients which might be of concern for products made by a company with poor quality controls but pose no concern for products made by a company with high quality control standards. In other words, they should not be spreading hysteria about the ingredient. They should focus on some of the real quality control issues in our industry.
To help you sort through all the hysteria about product ingredients, I have previously published a two-part series on ingredients in which I sorted through the claims and divided common ingredients into the good, the bad, and the ugly.
#6: Demand Proof
 This is the most important tip of all. Many companies make wild claims about their products but feel no need to back up their claims. Ignore their hype and demand they give proof to back up their claims.
This is the most important tip of all. Many companies make wild claims about their products but feel no need to back up their claims. Ignore their hype and demand they give proof to back up their claims.
- If they claim their products are pure, ask how many quality control tests they run on their products.
- If they claim their products work, ask for proof. Ask for clinical studies…
-
- That have been done with people, not with animals, cell culture, or test tubes*
-
- That have been published in peer-reviewed scientific journals.
-
- That have been done with their product, not studies done with another product.
*Animal, cell culture and test tube studies are valid if they are used to identify a potential mechanism of action but should not be cited as proof the product works. For ethical reasons, I prefer companies that do not use animal studies.
The Bottom Line
Everyone would like to get the best multivitamin-multimineral for their health at the least possible cost. However, there are lots of multivitamin-multimineral products in the marketplace. The pressure to win market share is intense. Quality controls and clinical studies are expensive. All too often companies try to differentiate their multivitamin-multimineral products based on marketing hype.
With so many claims and counter claims in the marketplace, it has become almost impossible for the average consumer to know how to choose the best multivitamin-multimineral product. In this week’s article, I have given you 6 tips you can use to select the multivitamin-multimineral product that is best for you. I have told you what to look for in a good multivitamin and which marketing claims you should just ignore. In summary:
- Start with the nutrition label. A good multivitamin-multimineral supplement should contain all 24 essential nutrients recommended by the Food and Nutrition Board of the Institute of Medicine (23 if the supplement is without iron). Anything else is probably marketing hype.
- Make sure the nutrients are in the correct balance. Again, your evaluation should be guided by the Institute of Medicine.
- Don’t fall for the hype. Many companies claim that they use a more natural, safer, or better utilized form of certain vitamins or minerals than their competitors. Ignore those claims. They are usually just marketing hype
- Don’t fall for buzz words. Some companies attempt to differentiate their products by claiming they are natural, organic, non-GMO, or are made from food. The companies are attaching buzz words to their product that they know resonate with the American people. Don’t believe them. Those claims are all bogus. They do nothing to improve your health. They are marketing hype.
- Don’t fall for scare tactics. Some companies try to scare you into buying their products by claiming their competitors are using unsafe ingredients. These claims are usually bogus.
- Demand poof. This is the most important tip of all. Many companies make wild claims about their products but feel no need to back up their claims. Ignore their hype and demand they give proof to back up their claims.
- If they claim their products are pure, ask how many quality control tests they run on their products.
- If they claim their products work, ask for proof. Ask for clinical studies…
-
- That have been done with people, not with animals, cell culture, or test tubes.
-
- That have been published in peer-reviewed scientific journals.
-
- That have been done with their product, not studies done with another product.
For more details about each of those tips, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 45 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.