The Lies Of The Supplement Industry
Author: Dr. Stephen Chaney

How do the myths of the food supplement industry originate? Some of them start innocently enough. They are often based on a kernel of truth which is misinterpreted by some well-meaning medical doctors.
It’s not their fault. We teach future doctors what I call “metabolism light” in medical school. There simply isn’t room in the medical curriculum to teach all the details and nuances of human metabolism.
We also try to teach them the basics of how to interpret scientific literature. However, it takes years of experience to get good at picking out the strengths and weaknesses of clinical studies.
The doctors form their hypothesis and test it on a few patients. If it works, they publish a paper. At that point their idea is picked up by the “sensationalist” bloggers. These are the bloggers who like to focus on the sensational. They delight in writing about “new findings” that go against what the medical profession has been telling you for years.
The bloggers don’t stop there. They usually expand the claims. They ‘cherry pick” the scientific literature by quoting only studies that support their viewpoint and ignoring studies that refute it. In short, they put together a very compelling story. Soon the story is picked up by other bloggers who embellish it further. After it appears in enough sites, people start believing it. A myth is born.
Then supplement companies get in the act. They sense there is money to be made. They manufacture supplements to provide nutrients supported by the myths. They embellish the mythology even more and put together a compelling story to market their products.
This is where the mythology becomes deception. Companies have the responsibility to design their products based on the best science. They have an obligation to tell the truth about their products. When they make claims they know cannot be true, they are lying to you.
The saga of methylfolate is a perfect example of how observations based on a kernel of truth became myths and eventually became downright lies. Let me share that story with you.
The Kernel Of Truth About Methylfolate
Let’s start with one of the “kernel of truth” that launched the whole methyl folate saga. It started with a doctor who was having a very difficult time finding a solution for a patient with some significant health issues. The doctor ordered a genetic test and discovered the patient had a deficiency in the methylene tetrahydrofolate reductase (MTHFR) gene.
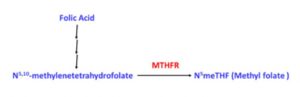 The doctor remembered the reaction catalyzed by MTHFR, and a light bulb went off. “Eureka”, he said. His patient must be unable to make N5-methyltetrahydrofolate (commonly referred to as methylfolate or methyl folate), and methylfolate is required for some very important methylation reactions in the cell.
The doctor remembered the reaction catalyzed by MTHFR, and a light bulb went off. “Eureka”, he said. His patient must be unable to make N5-methyltetrahydrofolate (commonly referred to as methylfolate or methyl folate), and methylfolate is required for some very important methylation reactions in the cell.
He gave his patient methylfolate, and the patient’s symptoms got better. The doctor leapt to the conclusion that other patients with MTHFR deficiency needed methylfolate as well. Many of those patients responded to methylfolate as well. He didn’t bother to check whether they responded equally well to folic acid. He just assumed methylfolate was the magic elixir.
He wrote a paper on his clinical observations, and the methylfolate story was launched. It all seemed so logical.
However, the story was not nearly as straight forward as the doctor and the people publicizing his findings assumed. Let me walk you through some “Metabolism 101”. Don’t worry. There won’t be a quiz.
Why The Original Assumptions About Methylfolate Were Misleading
MTHFR mutants only have a partial loss of activity.
- Individuals with 2 copies of a mutation from A to C at position 1298 of the MTHFR gene (A1298C homozygotes) comprise about 5% of the US population. They have 60% enzyme activity and appear to be normal in clinical studies.
- Individuals with 2 copies of a mutation from C to T at position 677 of the MTHFR gene (C677T homozygotes) have 30% enzyme activity. They comprise about 10% of the US population. C677T homozygotes often have elevated homocysteine levels. The homozygous C677T mutation is associated with depression, anxiety, and mood swings in some people, but not in others (I will come back to the significance of that qualifying statement later).
- C677T heterozygotes (one mutant gene) have 65% activity and are normal.
We Don’t Need 100% MTHFR Activity
 Our human body is wonderfully designed. For many of our most essential metabolic reactions we have built in redundancy. We don’t require 100% activity of key enzymes. This helps protect us from bad effects of mutations as they arise.
Our human body is wonderfully designed. For many of our most essential metabolic reactions we have built in redundancy. We don’t require 100% activity of key enzymes. This helps protect us from bad effects of mutations as they arise.
The best analogy I can think of is the US space program. Most space vehicles had built in redundancy so that if one system failed, the mission could go on. For example, you may remember the Hubble space telescope. It was launched with four gyroscopes to keep the telescope pointed in the right direction.After a few years, one gyroscope gave out. That was not a problem because there were three left. A few years later the second gyroscope gave out. Again, there was no problem because there were still two gyroscopes left.
It was only after the third gyroscope gave out that Hubble became a bit “wonky”, and a space shuttle was sent up to replace the gyroscopes. It is the same with MTHFR. Only when you get down to around 30% activity, does it become a bit wonky”. (That’s about as non-technical as I get.)
Not Everyone With MTHFR Deficiency Experiences Symptoms
This is due to a phenomenon my geneticist friends refer to as penetrance. Simply put, that means that not everyone with the same mutation experiences the same severity of symptoms. That is because the severity of a mutation is influenced by diet, lifestyle, and genetic background.
Let me start with genetic background. In terms of MTHFR mutants you can think of genetic background as being mutations in a related methylation pathway. People who have a mutation in both MTHFR and a gene in a related pathway will experience more severe symptoms and are more likely to require methylfolate. Once you understand penetrance, you realize that individuals requiring methylfolate may represent only a small subset of people with MTHFR mutations.
Penetrance is a concept that most proponents of the methylfolate hypothesis completely ignore. The most severe MTHFR mutation (C677T homozygote) increases the probability that individuals will exhibit symptoms, but some individuals with that mutation are completely normal. Now that you understand the concepts of redundancy and penetrance, you can understand why that is.
When Did The Kernel of Truth Become A Myth?
Up to this point the hype around methylfolate could be chalked up to an honest misunderstanding.
- The doctors who published the original papers may not have known that MTHFR mutations only resulted in a partial reduction in enzyme activity.
- They probably didn’t know the concepts of redundancy (our cells don’t need 100% enzyme activity) or penetrance (the same mutation may cause severe symptoms in some patients and have no effect in others).
- It seemed logical to assume that everyone with a MTHFR mutation might do better with methylfolate supplementation. That was incorrect, but it was an honest mistake.
 However, the message was picked up by the bloggers who specialize in sensational stories, especially stories that contradict what experts have been telling you for years. They picked up the methylfolate story and distorted it beyond recognition.
However, the message was picked up by the bloggers who specialize in sensational stories, especially stories that contradict what experts have been telling you for years. They picked up the methylfolate story and distorted it beyond recognition.
- They knew that “natural” is a buzz word, so they told you that methylfolate was natural and folic acid is synthetic.
- They told you that methylfolate was better utilized than folic acid.
- They told you that methylfolate was more effective than folic acid.
- They told you folic acid was toxic. It was going to increase your risk of cancer.
- Suddenly, it was no longer about people with MTHFR deficiency. You were told that everyone should avoid folic acid and use methylfolate instead.
On the surface, these pronouncements should not have passed the “If it sounds too good to be true…” test, or in this case, the “If it sounds too bad to be true…” test. You were being asked to believe that folic acid, which has been in use for over 80 years and is backed by hundreds of studies showing it is safe and effective, was neither safe nor effective. You were asked to believe that the government was poisoning you by fortifying foods with folic acid.
However, to make their blogs sound more convincing, they listed clinical studies supporting their stories. The problem is they “cherry picked” the studies that supported their story and ignored the rest. Their bias was particularly outrageous when it came to the “story” that folic acid increases cancer risks. They ignored 10 or 20 studies showing no cancer risk and reported one suggesting it might increase risk. I call that deceptive.
Unfortunately, the myths created by the bloggers have been repeated often enough that many people now believe they are true. It is time for me to debunk the methylfolate myths.
The Methylfolate Myths
 Myth: Methylfolate is natural. It comes from whole food. Folic acid is synthetic.
Myth: Methylfolate is natural. It comes from whole food. Folic acid is synthetic.
Fact: Methylfolate is chemically synthesized from folic acid. It is physically impossible to extract enough from whole foods. Here are the facts:
- Methyfolate is only one of several naturally occurring folates in foods.
- The best food sources of folates are beans, leafy greens, and broccoli.
- To obtain the RDA of methyfolate for a single tablet you would need to start with 1 cup of lentils, two cups of cooked spinach, or 4 cups of broccoli.
- You do the math! It just isn’t possible.
Myth: Methylfolate is better utilized by the body than folic acid.
Fact: This claim is based on levels of methylfolate in the blood after taking supplements providing equivalent amounts of methylfolate and folic acid. However, methylfolate has no biological activity in our blood. The measurement that matters is total folate levels (methylfolate plus other folates) in our cells.
If you take equivalent amounts of folic acid and methylfolate, you end up with identical folate levels in your cells (B.J. Venn et al, The Journal of Nutrition, 132: 3333-3335, 2002) In short, there is no difference in our ability to utilize methylfolate and folic acid.
Myth: If you have a mutation in the MTHFR gene, folic acid isn’t effective.
 Fact: MTHFR slightly increases the need for folic acid (from 400 ug to between 600 and 800 ug), but multiple studies show that folic acid supplementation is effective in people with MTHFR mutations.
Fact: MTHFR slightly increases the need for folic acid (from 400 ug to between 600 and 800 ug), but multiple studies show that folic acid supplementation is effective in people with MTHFR mutations.
For example, homocysteine levels are easily measured and are a reliable indicator of methylfolate status.
- One study has shown that folic acid and methylfolate were equally effective at lowering plasma homocysteine in people who were MTHFR C677T homozygotes (P. Fohr et al, American Journal of Clinical Nutrition, 75: 275-282, 2002).
- That study also showed that folic acid was more effective than methylfolate at lowering homocysteine in people who were C677T heterozygotes and in people with normal MTHFR activity.
- Another study showed folic acid was just as effective as a diet providing equivalent quantities of folate from foods at lowering homocysteine levels in people with various MTHFR mutations (A. Ashfield-Watt et al, American Journal of Clinical Nutrition, 76: 180-186, 2002).
At present, lowering of homocysteine levels is the only indicator of methylfolate status for which methylfolate and folic acid have been directly compared. However, there are other studies suggesting that folic acid is likely to be effective for people with MTHFR defects. For example:
- Folic acid has been shown in multiple studies to be effective in preventing neural tube defects (M. De-Regil et al, Cochrane Database Systematic Reviews 2010 Oct 6;(10):CD007950. PMID: 20927767), which are highly associated with the C677T MTHFR gene defect.
- Three studies have shown that supplementation with folic acid, B12, and B6 slowed cognitive decline in older people with elevated homocysteine levels ( Durga et al, The Lancet, 369: 208-216, 2007; A.D. Smith et al, PLoS ONE 5(9): e12244. doi:10.1371/journal.pone.0012244, 2010; G. Douaud et al, Proceedings of the National Academies of Sciences, 110: 9523-9528, 2013).
- In contrast, the one study that substituted methylfolate for folic acid showed no effect (A. McMahon et al, New England Journal of Medicine, 354: 2764-2769, 2006).
 Myth: Folic acid causes cancer.
Myth: Folic acid causes cancer.
Fact: The few studies suggesting that folic acid supplementation might increase the risk of cancer were “outliers”. By that I mean they contradicted many other studies showing no increased risk.
Scientists are accustomed to this. We know that studies sometimes come up with conflicting results. In some cases, we can point to an error in experimental design or statistical analysis as the cause of the aberrant results.
In other cases, we never know the reason for the differences, so we go with the weight of experimental evidence (what the majority of studies show). The weight of evidence clearly supports the safety of folic acid,
However, that is not enough. If there is the slightest possibility that something causes cancer, we investigate it further. Consequently, the scientific community followed up with larger studies.
Those studies showed either reduced cancer risk or no difference in cancer risk with folic acid supplementation. None of the studies found any evidence that folic acid increased cancer risk. I have covered this in detail for folic acid and colon cancer risk in a previous issue of “Health Tips From The Professor”.
There have also been a couple of small studies suggesting that folic acid might increase the risk of prostate and breast cancer. Although these were small, individual studies, they have been widely hyped by the methylfolate advocates. Once again, the definitive study has been done (S.E. Vollset et al, The Lancet, 381: 1029-1036, 2013).
It was a meta-analysis of 13 placebo-controlled studies involving over 50,000 subjects. The results were clear cut. Folic acid supplementation caused no increase in overall cancer risk, and no increase in the risk of colon cancer, prostate cancer, breast cancer, or any other individual cancer. Moreover, the average dose of folic acid in those studies was 2 mg/day, which is 5 times the RDA.
Of course, the bloggers and the companies selling methylfolate supplements ignore the definitive studies showing folic acid does not increase cancer risk. The myths and lies continue.
Myth: Folic acid can mask a B12 deficiency.
Fact: True but irrelevant if you use a supplement with folic acid and B12 in balance.
The Lies Of The Supplement Industry
 If you are writing a blog, you are covered by “freedom of speech”. You can say whatever you want. It doesn’t have to be true. However, if you are a supplement manufacturer, you are held to a higher standard. Ignorance is no longer an excuse. You can no longer cherry pick the “facts” you like and ignore the rest. You are ethically obligated to research all the available literature and be guided by the best scientific evidence.
If you are writing a blog, you are covered by “freedom of speech”. You can say whatever you want. It doesn’t have to be true. However, if you are a supplement manufacturer, you are held to a higher standard. Ignorance is no longer an excuse. You can no longer cherry pick the “facts” you like and ignore the rest. You are ethically obligated to research all the available literature and be guided by the best scientific evidence.
Reputable companies have been guided by scientific evidence and have not jumped on the methylfolate bandwagon. They know folic acid is both safe and effective in a wide variety of clinical situations. They also know that, while methylfolate may be just as effective as folic acid, it has not been shown to be superior to folic acid for any clinical application.
They may offer a methylfolate option for people who believe they need it. But they make no claim that it is superior to their products containing folic acid.
Less reputable companies, however, sensed money to be made by capitalizing on the buzz around methylfolate. They repeated the myths of the bloggers and claimed their products were superior to others on the market. They call it marketing. I call it lying. They have an obligation to fact check their claims and only make claims that are true.
Let me give you an example. In preparing for this article, I looked at the claims of several companies that were promoting their methylfolate supplements. One in particular claimed they had studies showing:
- Their methylfolate supplement was effective at reducing the risk of adverse pregnancy outcomes.
- Their methylfolate supplement was twice as bioavailable as folic acid.
- Their methylfolate supplement was able to lower homocysteine levels better than conventional folic acid supplementation.
All three studies were bogus.
- With respect to the first study, it was likely true that their methylfolate supplement decreased adverse pregnancy outcomes. But there are dozens of studies showing that folic acid does the same thing.
And because they did not compare methylfolate and folic acid supplementation in their studies, they have no basis for claiming their supplement was superior.
- The second study compared levels of methylfolate and folic acid in the blood. As I mentioned above, methylfolate has no biological activity in our blood. The measurement that matters is total folate levels (methylfolate plus other folates) in our cells. And previous studies have shown that equivalent amounts of methylfolate and folic acid give identical amounts of methyfolate in our cells.
- The third study compared their supplement, which contained B6, B12, zinc, and betaine in addition to methylfolate, to folic acid alone. That’s comparing apples to oranges. That is because there are three pathways for lowering homocysteine levels, and B6, B12, and betaine play important roles in each of these pathways.
-
- B12 is an integral part of the enzyme methionine synthase, an enzyme that converts homocysteine to the amino acid methionine. Methylfolate transfers its methyl group to the enzyme-bound vitamin B12, and methyl B12 transfers the methyl group to homocysteine, which converts it to methionine. In other words, methylfolate cannot lower homocysteine levels by itself. It needs vitamin B12.
-
- Betaine also serves as a methyl donor in another pathway for converting homocysteine to methionine by an enzyme called betaine-homocysteine methyltransferase.
-
- B6 is essential for yet another pathway that lowers homocysteine levels by converting homocysteine to the amino acid cysteine.
You might argue that the company was simply ignorant of the importance of B6, B12, and betaine for lowering homocysteine levels. However, that is unlikely. Why else would they have included B6, B12, and betaine in their supplement?
They must have known the study they designed was bogus. That suggests they conducted the study with the sole purpose of deceiving you, the consumer. I call that lying.
Finally, in case you were wondering, I am not recommending you select a single supplement with folic acid, B6, and B12. I do recommend you get your folic acid from a multivitamin or B complex supplement that provides all three B vitamins in balance.
Betaine deficiency is very rare, so I don’t include betaine in my recommendations.
What Does This Mean For You?
 MTHFR mutations only result in partial loss of activity. Most individuals with MTHFR defects remain symptom free with the RDA, or slightly above the RDA, of folic acid.
MTHFR mutations only result in partial loss of activity. Most individuals with MTHFR defects remain symptom free with the RDA, or slightly above the RDA, of folic acid.
However, there may be some individuals with a MTHFR defect and additional gene defects in metabolic pathways involving methylation who might benefit from methylfolate. This is due to a phenomenon that geneticists call penetrance and would likely represent a small subset of the population with MTHFR defects.
Finally,the claims that everyone would benefit from methylfolate instead of folic acid are false. They are contradicted by human metabolism and multiple published clinical studies.
In short, folic acid has been used for over 80 years. There are hundreds of clinical studies showing it is safe and effective, even in most individuals with a MTHFR deficiency. I can’t tell you whether the companies selling methylfolate are ignorant of basic metabolism and the published studies refuting their claims or whether they are purposely trying to deceive the public—but neither is a good thing.
The Bottom Line
Some supplement manufacturers are claiming that methylfolate is more natural and more effective than the folic acid that has been used in supplements for the past 80 years. In this issue of “Health Tips From the Professor” I debunk the methylfolate myths used by the supplement manufacturers to sell their methylfolate products.
I can’t tell you whether the companies selling methylfolate are ignorant of basic metabolism and the published studies refuting their claims or whether they are purposely trying to deceive the public—but neither is a good thing.
For more specifics, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
_____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_____________________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry textbooks for medical students.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years. Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”. Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry textbooks for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.