The Unexpected Benefits of Omega-3s
Author: Dr. Stephen Chaney
 Omega-3s have become the latest “super food”. Wherever you get your news, you are constantly seeing articles about the latest “miracle results” obtained by adding omega-3s to your diet.
Omega-3s have become the latest “super food”. Wherever you get your news, you are constantly seeing articles about the latest “miracle results” obtained by adding omega-3s to your diet.
There is good evidence that omega-3s:
- Lower blood pressure.
- Reduce triglycerides (fatty particles in your bloodstream).
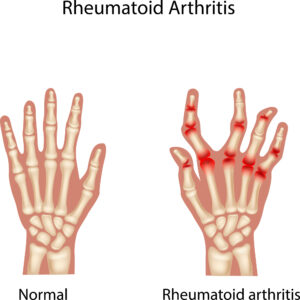
- Reduce chronic inflammation.
- Slow the buildup of plaque in the arteries (which combined with lowering blood pressure, reducing triglycerides, and reducing inflammation likely lowers heart disease risk).
- Reduce the risk of depression and anxiety.
- Improve neurodevelopment (cognitive function, memory, and learning) in infants and children.
- Reduce inflammation in joints.
In addition, omega-3s may:
- Reduce the risk of cognitive decline and Alzheimer’s as we age.
- Reduce the risk of arrhythmias (irregular heartbeats).
- Protect against age-related macular degeneration.
- Improve immune function.
- Reduce the risk of certain cancers.
- Improve blood sugar regulation.
Because obesity is associated with chronic inflammation and inflammation is associated with many of the health risks associated with obesity, the authors of the study I will be describing today (J Torres-Vanegas et al. Healthcare, 13:103, 2025) decided to look at the effect of supplementation with 1.8 grams of long-chain omega-3s (fish oil capsules) on the beneficial effects of a weight loss diet in a double-blind, placebo-controlled, 8 week study.
There were two interesting wrinkles to this study.
- Previous studies have suggested that a 5:1 ratio of omega-6 fats to omega-3 fats is optimal for these effects, but the typical American has an omega-6 to omega-3 ratio of between 15:1 and 20:1. So, the authors designed their study so that participants achieved a 5:1 omega-6 to omega-3 ratio.
- Because short-chain omega-3s (found in plant foods) have little effect on inflammation, they were used as the “active” placebo instead of omega-6 fats.
-
- In short, both groups received an omega-3 supplement. The “intervention” group received long-chain omega-3s from fish oil, and the “placebo control” group received short-chain omega-3s from vegetable oils (chia and flaxseed oil).
[Note: Short-chain omega-3s have many health benefits. However, their conversion to long-chain omega-3s in the human body is very inefficient, and they do not have all the health benefits associated with long-chain omega-3s.]
How Was This Study Done?
 The authors of this study enrolled 40 obese (BMI≥30) adults (40% females, 60% males), aged 30-50 in a randomized, active placebo-controlled, double-blind weight loss study for 8 weeks.
The authors of this study enrolled 40 obese (BMI≥30) adults (40% females, 60% males), aged 30-50 in a randomized, active placebo-controlled, double-blind weight loss study for 8 weeks.
The estimated caloric expenditure was determined for each participant prior to the study. Based on that estimate calories were reduced by 200 calories/day for the first 4 weeks and 400 calories/day for weeks 5-8.
Dietitians designed a recipe book of 3 main meals and 2 snacks for each day. The diets were designed to achieve the caloric restriction described above and to achieve a 5:1 ratio of omega-6 to omega-3.
Participants completed a 3-day food frequency questionnaire including 2 weekdays and 1 weekend day at the start of the study and at week 8. Participants were guided in this by a dietitian using food models to help them assess portion sizes.
Half of the participants were given a long-chain omega-3 supplement containing 1080 mg of EPA plus 720 mg of DHA (1,800 mg total) from fish oil. The other half of the participants were given a short-chain omega-3 supplement consisting of 1,600 mg of ALA from chia and flaxseed oil. The dietary assessments showed that both groups were successful in achieving a 5:1 omega-6 to omega-3 ratio when the supplements were included in the calculation.
Can Omega-3s Improve Weight Loss Diets?
 Because both groups had equal caloric restriction. Therefore, as expected, both groups experienced decreased:
Because both groups had equal caloric restriction. Therefore, as expected, both groups experienced decreased:
- Body weight.
- BMI.
- Percent body fat.
- Total cholesterol.
- Triglycerides.
- VLDL.
However, when the scientists measured markers of inflammation, a different picture was observed.
- IL-6 (Interleukin 6) and RvD1 (resolving D1) are inversely associated with inflammation (They increase when inflammation decreases).
-
- IL-6 and RVD1 increased only in the group supplementing with long-chain omega-3s (EPA + DHA).
- IL-10 and MCP-1 (monocyte chemoattractant protein-1) are directly associated with inflammation (They decrease when inflammation decreases).
-
- IL-10 and MCP-1 decreased only in the group supplementing with long-chain omega-3s.
- These differences were highly significant.
The authors concluded, “A diet supplemented with marine n-3 (long-chain omega-3s from fish oil) improves inflammatory markers by increasing systemic levels of Resolvin D1 and IL-10 and decreasing IL-6 and MCP-1.”
“These results could provide a guide for future nutritional intervention strategies aimed to…reduce chronic low-grade inflammation by considering the omega-6 to omega-3 ratio content as a necessary calculation for a proper diet.”
[I would note that both diets achieved an omega-6 to omega-3 ratio of 5:1, but only the diet containing long-chain omega-3s reduced inflammation. So, the author’s statement is only true for long-chain omega-3s.]
In short, weight loss is known to help reduce chronic inflammation. Both groups lost weight, but only the group supplementing with long-chain omega-3s had a significant improvement in inflammatory markers.
- These data suggest that supplementation with long-chain omega-3s while on a weight loss diet greatly enhances the reduction in inflammation associated with weight loss.
- These data also suggest that short-chain omega-3s do not significantly reduce inflammation.
- Both findings are consistent with earlier studies.
The Unexpected Benefits Of Omega-3s
- Abdominal obesity was reduced by 35% in the long-chain omega-3 group compared to 5.6% in the short-chain omega-3 group, and these differences were highly significant.
- Weight loss for men in the long-chain omega-3 group was 9.25 pounds compared to 4.8 pounds in the short-chain omega-3 group, and these differences were significant.
- Reductions in percent body fat and waist circumference were also greater for men in the long-chain omega-3 group, but these differences were not statistically significant in this small study.
In short, these data suggest that long-chain omega-3 supplementation may have enhanced weight loss. This is an intriguing finding that needs to be confirmed by future studies.
What Does This Study Mean For You?
 This study is a randomized, double-blind, placebo-controlled trial, which is the gold standard for clinical studies. But it is also a very small study, so we need to carefully consider the validity of the study.
This study is a randomized, double-blind, placebo-controlled trial, which is the gold standard for clinical studies. But it is also a very small study, so we need to carefully consider the validity of the study.
It had three major findings.
#1: Omega-3s enhance the anti-inflammatory effect of weight loss diets.
#2: This effect is only seen for the long-chain omega-3s EPA and DHA found in fish oil. The short-chain omega-3 ALA found in vegetable oils and other plant foods had no significant effect on inflammation.
The anti-inflammatory effect of long-chain omega-3s and the lack of an effect of short-chain omega-3s on inflammation are consistent with many previous studies. The only novel aspect of this study was the finding that the same effects occurred when omega-3 supplementation was added to a weight loss diet.
That is an important consideration because many weight loss diets focus on plant foods or red meats. Fish are often missing from the diet plan and long-chain omega-3 supplementation is seldom recommended.
That’s unfortunate because chronic inflammation is associated with obesity. And chronic inflammation increases the risk of heart disease, diabetes, cancer, and all the “itis” diseases. Omega-3 supplementation should be an important part of any weight loss diet.
#3: This study also suggests that long-chain omega-3 supplementation may increase the effectiveness of weight loss diets.
At this point I consider this finding as possible, but not probable. Previous studies have reported conflicting results. Some studies have suggested omega-3s aid weight loss. Others have found no effect.
We need many more studies before I would be ready to recommend omega-3 supplementation as an aid to weight loss. However, omega-3s have many proven benefits. If they also happen to make weight loss diets more effective, this would be an unexpected benefit.
The Bottom Line
A recent study looked at the effect of omega-3 supplementation during a weight loss diet. The study had three main findings.
#1: Omega-3 supplementation enhances the anti-inflammatory effect of weight loss diets.
#2: This effect is only seen for the long-chain omega-3s EPA and DHA found in fish oil. The short-chain omega-3 ALA found in vegetable oils and other plant foods had no significant effect on inflammation.
#3: This study also suggests that long-chain omega-3 supplementation may increase the effectiveness of weight loss diets.
For more information on this study and what it means for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
____________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
____________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.