Do You Need A Magnesium Supplement?
Author: Dr. Stephen Chaney
 Getting an adequate amount magnesium from our diet should not be a problem. Magnesium is found in a wide variety of foods with the best sources being legumes (beans), nuts, seeds, whole grains, green leafy vegetables, and dairy foods.
Getting an adequate amount magnesium from our diet should not be a problem. Magnesium is found in a wide variety of foods with the best sources being legumes (beans), nuts, seeds, whole grains, green leafy vegetables, and dairy foods.
The problem is:
- None of these foods contain enough magnesium by themselves to provide the RDA (420 mg/day for men and 320 mg/day for women) for magnesium. We need to consume a variety of these foods every day – something most Americans aren’t doing.
- These foods are decent sources of magnesium only in their unprocessed form. And most Americans consume more highly processed foods than whole, unprocessed foods.
- Two to three servings of dairy provide a decent amount of magnesium, but many Americans are cutting back on dairy. And plant-based dairy substitutes often provide much less magnesium than the dairy food they replace.
- Finally, green leafy vegetables (iceberg lettuce doesn’t count) don’t make it into the American menu as often as they should.
As a result, recent studies find that at least 50% of Americans are not getting enough magnesium in their diet. In fact, the average magnesium intake in this country is 268 mg/day for men and 234 mg/day for women. And the figures are not very different in other developed countries.
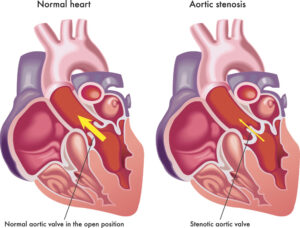
Does it matter? Recent studies have shown that an adequate intake of dietary magnesium is associated with lower risks of cardiovascular diseases (CVD) and all-cause mortality. This may be because of the of role of magnesium in supporting heart muscle contraction, normal heart rhythm, and blood pressure regulation. Adequate magnesium intake is also associated with lower risk of type 2 diabetes.
But what if you have already had a heart attack? Is it too late for magnesium to make a difference? A recent study (I Evers et al, Frontiers in Cardiovascular Medicine, August 12, 2022) was designed to answer this question.
The authors examined the effect of magnesium intake on cardiovascular disease (CVD) mortality, all-cause mortality, and coronary heart disease (CHD) mortality in patients who had experienced a recent heart attack.
[Note: CHD is defined as heart disease due to clogged coronary arteries, such as a heart attack. CVD includes CHD plus diseases caused by other clogged blood vessels, such as strokes and peripheral artery disease].
How Was The Study Done?
 The authors used data from a previous study that had enrolled 4,365 Dutch patients aged 60-80 (average age = 69) who had experienced a heart attack within approximately 4 years prior to enrollment and followed them for an average of 12.4 years. All patients were receiving standard post-heart attack drug therapy.
The authors used data from a previous study that had enrolled 4,365 Dutch patients aged 60-80 (average age = 69) who had experienced a heart attack within approximately 4 years prior to enrollment and followed them for an average of 12.4 years. All patients were receiving standard post-heart attack drug therapy.
The characteristics of the patients enrolled in the study were as follows:
- Male 79%, female 21%
- Average magnesium intake = 302 mg/day
- Percent magnesium deficient: 72% of men and 67% of women
- Percent taking magnesium supplements = 5.4%
- Percent on drugs to lower blood pressure = 90%
- Percent on statins = 86%
- Percent on diuretics = 24%
Upon entry into the study the patients were asked to fill out a 203-item food frequency questionnaire reflecting their dietary intake over the past month. Trained dietitians reviewed the questionnaires and phoned the participants to clarify any unclear or missing items. The questionnaires were linked to the 2006 Dutch Food Composition Database to calculate magnesium intake and other aspects of their diets.
The patients were divided into 3 groups based on their energy adjusted magnesium intakes and those in the highest third (>322 mg/day) were compared to those in the lowest third (<238 mg/day) with respect to cardiovascular disease (CVD), all-cause mortality, and coronary heart disease (CHD) mortality.
The comparisons were statically adjusted for fiber intake (most magnesium-rich foods are also high fiber foods), diuretic use (diuretics reduce magnesium levels in the blood), age, sex, smoking, alcohol use, physical activity, obesity, education level, caloric intake, calcium, vitamin D, sodium from foods, potassium, heme iron, vitamin C, beta-carotenoids, polyunsaturated fatty acids, saturated fatty acids, overall diet quality based on the Dutch Dietary Guidelines, systolic blood pressure, kidney function, and diabetes. In other words, the data were adjusted for every conceivable variable that could have influenced the outcome.
Does Magnesium Protect Your Heart?
 When those with the highest magnesium intake (>322 mg/day) were compared to those with the lowest intake (<283 mg/day):
When those with the highest magnesium intake (>322 mg/day) were compared to those with the lowest intake (<283 mg/day):
- Cardiovascular disease (CVD) mortality was reduced by 28%.
- All-cause mortality was reduced by 22%.
- Coronary heart disease (CHD) mortality was reduced by 16%, but that reduction was not statistically significant.
They then looked at the effect of some variables that might affect CVD risk on the results.
- Diabetes, kidney function, iron intake, smoking, alcohol use, blood pressure, most dietary components and overall diet quality had no effect on the results.
- The results were also not affected when patients using a magnesium supplement were excluded from the analysis. This suggests the effect of magnesium from diet and supplementation is similar.
- However, diuretic use had a significant effect on the results.
-
- For patients using diuretics, high magnesium intake versus low magnesium intake reduced CVD mortality by 45%.
How Much Magnesium Do You Need?
 You may have noticed that the difference between the highest magnesium intake group and the lowest intake group was, on average, only 39 mg/day. So, the authors also used a statistical approach that utilized data from each individual patient to produce a graph of magnesium intake versus risk of CVD, total, and CHD mortality. For all 3 end points the graphs showed an inverse, linear relationship between magnesium and mortality.
You may have noticed that the difference between the highest magnesium intake group and the lowest intake group was, on average, only 39 mg/day. So, the authors also used a statistical approach that utilized data from each individual patient to produce a graph of magnesium intake versus risk of CVD, total, and CHD mortality. For all 3 end points the graphs showed an inverse, linear relationship between magnesium and mortality.
From this, the authors were able to calculate the effect of each 100mg/day increase in magnesium intake on mortality risk. Each 100mg/day of added magnesium reduced the risk of:
- CVD mortality by 38%.
- All-cause mortality by 30%.
- CHD mortality by 33%, and these results were borderline significant.
The inverse relationship between magnesium intake was observed at intakes ranging from around 200 mg/day to around 450 mg/day, which represented the range of dietary magnesium intake in this Dutch population group.
This study did not define an upper limit to the beneficial effect of magnesium intake because the graphs had not plateaued at 450 mg/day, suggesting that higher magnesium intakes might give even better results.
The authors concluded, “We observed a strong, linear inverse association of dietary magnesium with CVD and all-cause mortality after a heart attack, which was most pronounced in patients who used diuretics. Our findings emphasize the importance of an adequate magnesium intake in CVD patients, on top of cardiovascular drug treatment.”
I might add that this is the first study to look at the effect of magnesium on long-term survival after a heart attack.
Do You Need A Magnesium Supplement?
 As I said earlier, the best dietary sources of magnesium are beans, nuts, seeds, whole grains, green leafy vegetables, and dairy foods. And:
As I said earlier, the best dietary sources of magnesium are beans, nuts, seeds, whole grains, green leafy vegetables, and dairy foods. And:
- None of these foods contain enough magnesium by themselves to provide the RDA (420 mg/day for men and 320 mg/day for women) for magnesium.
- These foods are decent sources of magnesium only in their unprocessed form.
When unprocessed, each of these foods provides 20 to 60 mg of magnesium per serving. If we use an average value of 40 mg/serving, you would need in the range of 8-10 servings/day of these foods in their unprocessed form to meet the RDA for magnesium.
You could get a more accurate estimate of the magnesium content of your diet using the “Magnesium Content of Selected Foods” table from the NIH Factsheet on Magnesium.
Now you are ready to ask yourself two questions:
- Does my current diet provide the RDA for magnesium?
2. If not, am I willing to make the dietary changes needed to increase my magnesium levels to RDA levels?
If your answer to both questions is no, you should probably consider a magnesium supplement. A supplement providing around 200 mg of magnesium should bring all but the worst diets up to the recommended magnesium intake.
The current study did not define an upper limit for the beneficial effect of magnesium on survival after a heart attack but suggested that intakes above 450 mg/day might be optimal.
I do not recommend megadoses of magnesium, but intakes from diet and supplementation that slightly exceed the RDA appear to be safe. In their Magnesium Factsheet, the NIH states, “Too much magnesium…does not pose a health risk in healthy individuals because the kidneys eliminate excess amounts in the urine.”
The only concern is that magnesium from supplements is absorbed much more rapidly than magnesium from foods, and this can cause gas, bloating, and diarrhea in some individuals. For this reason, I recommend a sustained release magnesium supplement, so the magnesium is absorbed more slowly.
Finally, we should not consider magnesium as a magic bullet. The current study statistically eliminated every known variable that might affect survival after a heart attack, so it could estimate the beneficial effects of magnesium alone.
However, survival after a heart attack will likely be much greater if diet, exercise, and body mass are also optimized.
The Bottom Line
Recent studies have shown that an adequate intake of dietary magnesium is associated with lower risks of cardiovascular diseases (CVD) and all-cause mortality.
But what if you have already had a heart attack? Is it too late for magnesium to make a difference? A recent study of heart attack patients in Holland was designed to answer this question.
The authors examined the effect of magnesium intake on cardiovascular disease (CVD) mortality, all-cause mortality, and coronary heart disease (CHD) mortality in patients who had experienced a recent heart attack.
When heart attack patients with the highest magnesium intake (>322 mg/day) were compared to those with the lowest intake (<283 mg/day):
- Cardiovascular disease (CVD) mortality was reduced by 28%.
- All-cause mortality was reduced by 22%.
- Coronary heart disease (CHD) mortality was reduced by 16%, but that reduction was not statistically significant.
The authors went on to look at the inverse linear relationship between magnesium intake and mortality risk. They found that each 100mg/day of added magnesium reduced the risk of:
- CVD mortality by 38%.
- All-cause mortality by 30%.
- CHD mortality by 33%, and these results were borderline significant.
The authors concluded, “We observed a strong, linear inverse association of dietary magnesium with CVD and all-cause mortality after a heart attack…Our findings emphasize the importance of an adequate magnesium intake in CVD patients…”
I might add that this is the first study to look at the effect of magnesium on long-term survival of patients who have suffered a heart attack.
For more details on this study and my discussion of whether you might benefit from a magnesium supplement, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure, or prevent any disease.