Is There an American Omega-3 Deficiency?
Author: Dr. Stephen Chaney
 Omega-3s have been controversial in recent years. However, virtually everyone agrees that omega-3 intake in North American is low. But, would you believe that the United States and Canada are dead last with respect to omega-3 status – that we are among the countries with the lowest omega-3 status in the world? Is there an American omega-3 deficiency? That is what a recent study suggests!
Omega-3s have been controversial in recent years. However, virtually everyone agrees that omega-3 intake in North American is low. But, would you believe that the United States and Canada are dead last with respect to omega-3 status – that we are among the countries with the lowest omega-3 status in the world? Is there an American omega-3 deficiency? That is what a recent study suggests!
Omega-3 Deficiency in Americans
Previous studies have suggested that the American and Canadian diets were deficient in long chain omega-3s like EPA and DHA, but those studies were based on 24-hour diet recalls or food frequency surveys which might underrepresent the true amount of omega-3s in the diet. Therefore, a group of investigators from the United States and Canada decided to look at blood levels of EPA and DHA.
This study (Stark et al, Progress In Lipid Research, 63: 132-152, 2016) was a meta-analysis of 298 studies that recorded blood levels of EPA and DHA. These studies were from 36 counties and distinct regions around the world. They converted all of the measurements to a common unit expressed as percent by weight of EPA + DHA relative to the total weight of fatty acids in the blood.
 They combined all studies from a given country or region to give an average value of percent EPA + DHA and then divided the countries and regions into four groupings based on the average weight percentage of EPA + DHA in the blood. If all that seems confusing, the figure on the right (taken from Stark et al, Progress In Lipid Research, 63: 132-152, 2016) should clear things up.
They combined all studies from a given country or region to give an average value of percent EPA + DHA and then divided the countries and regions into four groupings based on the average weight percentage of EPA + DHA in the blood. If all that seems confusing, the figure on the right (taken from Stark et al, Progress In Lipid Research, 63: 132-152, 2016) should clear things up.
- Red = very low (< 4%) EPA + DHA levels
- Orange = low (4-6%) EPA + DHA levels
- Yellow = moderate (6-8%) EPA + DHA levels
- Green = adequate (>8%) EPA + DHA levels
- Grey = no valid measurements in those countries
It is clear from this study that most Americans and most Canadians don’t do a very good job of incorporating omega-3 fatty acids into their diet, as several previous dietary surveys have suggested. This could contribute to omega-3 deficiency.
Is The United States Dead Last In Omega-3 Status?
The global map of EPA + DHA blood levels certainly suggests that the United States is among a handful of countries with the very lowest omega-3 status. There are a few caveats, however.
- As the large areas of grey indicate, there are a number of countries with no valid omega-3 blood measurements. The United States might have lots of company in the very low omega-3 status category.
- There are some very large countries like Russia which have relatively few omega-3 blood measurements, and those measurements are only from a few regions of the country. The average omega-3 status for the entire country might be lower than indicated in this map.
On the other hand, there are lots of omega-3 blood measurements from countries like Japan, so it is clear that there are countries with much better omega-3 status than the United States.
What Does This Study Mean To You?
The important questions are, of course:Does it matter? What do these blood levels of EPA + DHA actually mean? Is < 4% EPA + DHA low enough to matter? What are the health consequences of low omega-3 status? If you have an omega-3 deficiency, what are the risks?
Let’s start with the first question: How do we translate a blood level of EPA + DHA into how much we should be getting in our diet? While there is no established Dietary Reference Intake for EPA + DHA, several expert panels and international organizations have made recommendations for EPA + DHA intake. Those recommendations generally range from 250 mg/day to 500 mg/day for general health and 500 mg/day to 1,000 mg/day for heart health. Unfortunately, most people in the United States and Canada consume less than 200 mg/day of omega-3 fatty acids, and most of those are short chain omega-3s that are inefficiently converted to the long chain EPA and DHA.
More importantly, a recent study (Patterson et al, Nutrition Research, 35: 1040-1051, 2015) has examined how much additional EPA + DHA must be consumed by someone eating a typical North American diet to significantly improve their omega-3 status. It showed that:
- 200 mg/day of EPA + DHA is required to improve omega-3 status from very low to low.
- 500 mg/day of EPA + DHA is required to improve omega-3 status from very low to moderate.
- 1250 mg/day of EPA + DHA is required to improve omega-3 status from very low to adequate.
 It is no surprise that these numbers correlate so well. My recommendation would be to consume at least 500 mg/day of EPA + DHA for general health and at least 1,000 mg/day for heart health.
It is no surprise that these numbers correlate so well. My recommendation would be to consume at least 500 mg/day of EPA + DHA for general health and at least 1,000 mg/day for heart health.
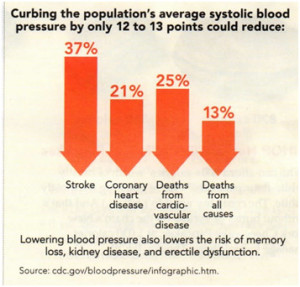
Now let’s look at the last question: What are the health consequences of low omega-3 status? There are multiple health benefits associated with optimal omega-3 status, but the best evidence is for the beneficial effects of omega-3s on fetal and infant neurodevelopment and heart health. For example:
- A recent meta-analysis conducted by scientists at Tufts and Harvard (Shulkin et al, The FASEB Journal, 30: supplement 295-6, 2016) concluded that DHA + EPA supplementation during pregnancy and infancy improved motor skills. Other studies have suggested that DHA + EPA supplementation in infancy and childhood improves reading skills and reduces ADHD symptoms in children with low omega-3 status.
- Several major clinical studies have shown that oily fish and fish oil supplements improve heart health and reduce the risk of heart attacks in at-risk individuals (Investigators of the GISSI-Prevenzione trial, Lancet, 354: 447-455, 1999 (http://www.thelancet.com/pdfs/journals/lancet/PIIS0140-6736(99)07072-5.pdf); Lamaitre et al, American Journal of Clinical Nutrition, 77: 319-325, 2003 (http://ajcn.nutrition.org/content/77/2/319); Gammelmark et al, British Journal of Nutrition, 116: 167-177, 2016 (http://journals.cambridge.org/action/displayAbstract?fromPage=online&aid=10341239&fileId=S000711451600180X).
- In case you have been confused by recent studies suggesting that omega-3s have no effect on heart health you should know that most of those studies were looking at the effect of EPA + DHA in patients who were already taking 3 or 4 heart medications. The studies actually concluded omega-3s provided no additional benefits in people already taking multiple heart medications. That is a totally different question.
Where Should You Get Your Omega-3s?
 Now that you know how important the long chain omega-3s, EPA and DHA, are for your health, and you know that most of us have a very poor omega-3 status and therefore have an omega-3 deficiency , your next questions are likely to be: “What’s the best way to improve my omega-3 status?” and “Where can I find EPA and DHA in my diet?” The answer is complicated.
Now that you know how important the long chain omega-3s, EPA and DHA, are for your health, and you know that most of us have a very poor omega-3 status and therefore have an omega-3 deficiency , your next questions are likely to be: “What’s the best way to improve my omega-3 status?” and “Where can I find EPA and DHA in my diet?” The answer is complicated.
- Cold water, oily fish like salmon are a great source of EPA and DHA. Unfortunately, our oceans are increasingly polluted and some of those pollutants are concentrated even more in farm raised fish. A few years ago a group of experts published a report in which they analyzed PCB levels in both wild caught and farm-raised fish from locations all around the world (Hites et al, Science 303: 226-229, 2004) . Based on PCB levels alone they recommended that some wild caught salmon be consumed no more than once a month and some farm raised salmon be consumed no more than once every other month!
Unfortunately, when you buy salmon in the grocery store or your favorite restaurant, you can ask whether the salmon is wild or farm-raised, but you have no idea where the salmon came from. You have no idea how safe it is to eat. I love salmon and still eat it on occasion, but not nearly as frequently as I used to.
As an aside, the buzzword nowadays is sustainability. I support sustainability. However, the easiest way to assure that fish are sustainable is to raise them in fish farms. When a waiter tells me how sustainable the “catch of the day” is, I ask them how polluted it is. If they can’t answer, I don’t buy it. My health is more important to me than sustainability.
- Nuts, seeds, and canola oil are good sources of ALA, a short chain omega-3 fatty acid. These food sources are less likely to be contaminated, but the efficiency of conversion of ALA to EPA and DHA is only around 5-10%. In other words, you need to eat a lot of ALA-rich foods to enjoy the health benefits associated with EPA and DHA.
- That leaves fish oil supplements, but you need to remember that the EPA + DHA supplements you purchase in the health food store come from polluted fish. Unfortunately, many manufacturers have inadequate purification and quality control standards. In other words, neither you nor they know whether their omega-3 products are pure. You need to make sure that the omega-3 supplement you purchase is made by a manufacturer with stringent quality control standards.
The Bottom Line
- A recent study has shown that most Americans are deficient in long chain omega-3s like EPA and DHA. In fact, the mainland United States and Canada were tied with half a dozen other countries for the lowest omega-3 status in the world. Omega-3 deficiency in Americans seems to be the worst.
- That is unfortunate because recent studies have shown that optimal blood levels of EPA and DHA are associated with a number of health benefits, especially fetal and infant neurodevelopment and heart health.
- Other studies suggest that most Americans should consume an extra 500 mg/day of EPA + DHA for general health and at least 1,000 mg/day for heart health.
- Unfortunately, it is not easy get those levels of EPA and DHA from our diet:
- Oily, cold water fish are a great source of EPA and DHA, but our oceans are increasingly polluted and experts recommend that some fish that are the best sources of EPA and DHA be consumed no more than once a month. The situation is even worse for farm-raised fish.
- Of course, nowadays the buzzword for fish is sustainability, but sustainability does not guarantee purity. Sustainable fish can be just as polluted as the worst of the farm raised fish.
- seeds and canola oil are great sources for ALA, a short chain omega-3 fatty acid. This source of omega-3s is less likely to be contaminated, but the efficiency of conversion of ALA to EPA and DHA in our bodies is only around 5-10%.
- Fish oil supplements can be a convenient source of the EPA and DHA you need, but the fish oil often comes from polluted fish and many manufacturers have inadequate purification methods and quality control standards. If you choose fish oil supplements as your source of omega-3s, be sure to choose a manufacturer with stringent quality control standards. Otherwise, neither you nor the manufacturer will know whether their omega-3 supplement is pure.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.