
Subscribe To Our Newsletter And Get 2 Free eBooks
Our Mission
“Health Tips from the Professor” is dedicated to providing busy professionals with cutting edge health information in a way that is both scientifically accurate and understandable. Our goal is to keep you abreast of the latest developments in health, nutrition and fitness. We will cut through the sensational headlines and hype to let you know what information you can trust, and we will provide you with this information in a straight-forward manner so that you can apply it to your personal health goals.
Most Read Articles From Dr. Steve Chaney
Latest Article
Vitamin D Just Got More Complicated
Posted June 10, 2025 by Dr. Steve Chaney
The Hidden Flaws Of Vitamin D Studies
Author: Dr. Stephen Chaney
 If I can paraphrase a famous saying, the question is, “To D or not to D.” On the one hand, you are told that vitamin D is a miracle supplement. It cures all your ailments. On the other hand, you are told that vitamin D supplements are worthless. They are a waste of money.
If I can paraphrase a famous saying, the question is, “To D or not to D.” On the one hand, you are told that vitamin D is a miracle supplement. It cures all your ailments. On the other hand, you are told that vitamin D supplements are worthless. They are a waste of money.
The problem is that vitamin D studies are all over the map. Some have shown beneficial effects of vitamin D supplementation. Others have come up empty. That allows “experts” to cherry pick the studies that support their bias. No wonder you are so confused.
If you have read my books or previous issues of “Health Tips From the Professor”, you know there is no such thing as a perfect clinical study. They all have their flaws. Sometimes the flaws are obvious. But sometimes we never know the flaws. We just know those studies are outliers.
So, let’s delve a little deeper into vitamin D metabolism and the hidden flaws that may have prevented some studies from showing the benefits of vitamin D supplementation. Then we will look at new data suggesting that vitamin D supplementation is more complicated than anyone imagined.
A Vitamin D Primer
 Let’s start with a brief review of vitamin D metabolism.
Let’s start with a brief review of vitamin D metabolism.
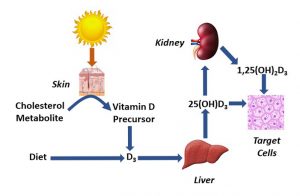
- Vitamin D metabolism starts in the skin when 7-dehydrocholesterol (a metabolite of cholesterol) is converted to cholecalciferol (vitamin D3) in a reaction requiring sunlight.
-
- In this sense, vitamin D3 is a hormone produced by the body. It only became an essential nutrient (vitamin) when Homo sapiens migrated to Northern latitudes and started to spend most of their time indoors.
- Vitamin D then travels to the liver where it is converted to 25-hydroxyvitamin D. This is the most abundant form of vitamin D in the blood.
- 25-hydroxyvitamin D next travels to the kidney where it is converted to 1,25-dihydroxyvitamin D. This is the active form of vitamin D. It is the form that binds to the vitamin D receptor.
Vitamin D was first discovered as an essential nutrient that was needed for adequate bone mineralization. It prevented rickets in children and osteomalacia in adults.
- The role of vitamin D in building strong bones is well established.
However, a few decades ago, it was discovered that vitamin D receptors were found in many other tissues including skin, immune system, heart, muscle, brain and nerves, and fat cells. This revolutionized our understanding of vitamin D’s role in the body.
- This led to suggestions that vitamin D played a role in immunity and autoimmune diseases, brain function and mood, heart health, muscle and fat metabolism, and much more. Here is where it started to get confusing.
-
- Some studies showed positive results. They found that vitamin D played an important role in each of these areas, and that vitamin D supplementation was beneficial
-
- Other studies showed negative results. They found no benefit of vitamin D supplementation.
So, the question arose, “Were the negative studies flawed?” In some cases, the answer was a clear, “Yes”. The flaws were easy to identify. In other cases, no obvious flaw could be discovered.
However, that has changed dramatically in recent years when some “hidden flaws” were discovered that invalidated many of the negative studies. That’s the topic of my next section.
The Hidden Flaws Of Vitamin D Studies
 Most previous studies simply measured vitamin D intake:
Most previous studies simply measured vitamin D intake:
- In dietary studies, vitamin D intake was measured using diet questionnaires.
- In supplement studies, vitamin D intake was measured by tracking whether the participants took all the supplement pills they were provided.
It was assumed that a certain dose of vitamin D produced the same blood levels of 1,25-dihydroxyvitamin D in everyone.
Now we know that assumption was flawed. The absorption and conversion of vitamin D to 1,25-dihydroxyvitamin D varies widely from individual to individual.
That means that every vitamin D study that relied on vitamin D intake without measuring its effect on blood 1,25-dihydroxyvitamin D levels is flawed. Their conclusions may or may not be true. Their evidence is unreliable.
I’m willing to give the authors of these studies some grace. They didn’t purposely design a flawed study. At the time they designed their studies we didn’t know about individual variability in the conversion of vitamin D to 1,25-dihydroxyvitamin D.
However, there is another “hidden flaw” I’m less willing to excuse. There have been some recent papers that measured 1,25-dihydroxyvitamin D levels before and after supplementation and have concluded that vitamin D supplementation had no benefit.
However, they failed to mention that the group they were studying already had adequate 1,25-dihydroxyvitamin D levels in their blood prior to supplementation. Under those circumstances there is no reason to expect that vitamin D supplementation will have any significant benefit.
This is an obvious flaw. But I call it a “hidden flaw” because the authors hid it. They didn’t mention it in their abstract or conclusion.
That’s dishonest. Most people just read the abstract and conclusions, and that is the information that is shared in the media. Very few people read the study to see if the abstract and conclusions are accurate.
As if this weren’t complicated enough, our understanding of the effects of vitamin D just got a lot more complicated.
Vitamin D Just Got More Complicated
 Two recent reports indicate that predicting who will benefit from vitamin D supplementation may be even more complicated than we thought.
Two recent reports indicate that predicting who will benefit from vitamin D supplementation may be even more complicated than we thought.
Report #1 suggests that there is significant individual variability in how people respond to blood levels of 1,25-dihydroxyvitamin D. If true, this adds another level of complexity to studies of vitamin D supplementation.
- Not only do the studies need to measure the 1,24-dihydroxyvitamin D levels before and after supplementation for everyone in the study.
- But they would also need to measure the individual response to 1,25-dihydroxyvitamin D.
This report (C Carlberg and A Haq, Journal of Steroid Biochemistry & Molecular Biology, 175: 12-17, 2018) summarized the results of two clinical studies and used that information to develop what they called the, “Personal Vitamin D Response Index”.
- The first study supplemented elderly men (average age = 71) for 5 months during the Finnish winter (when blood 1,25-dihydroxyvitamin D levels are lowest) with 0, 1600 IU, or 3200 IU per day.
- The second study supplemented young (average age = 35) men and women with a single high dose of vitamin D (80,000 IU) and followed them for 30 days.
At the beginning and end of each study:
- Blood levels of 1,25-dihydroxyvitamim D were measured.
- The activity of 24 vitamin D-responsive genes was measured. (These are genes whose activity is controlled by a vitamin D receptor and whose activity was known to respond to vitamin D.)
- In addition, more than 100 clinical and biochemical parameters that might be affected by vitamin D levels were measured. Of these, 12 were found to respond to vitamin D supplementation.
The authors of this report combined all 36 vitamin D-responsive biomarkers (24 genes and 12 biochemical parameters) into a single screening panel they called the “personal vitamin D response index” and correlated this index with the change in 25-dihydroxyvitamin D levels for each individual.
They discovered significant individual variability in how the subjects in these studies responded to increases in their 1,25-dihydroxyvitamin D levels. For example:
- They were able to divide the study participants into low, mid, and high responders to an increase in 1,25-dihydroxyvitamin D levels.
-
- In the first study 23.9% were low responders, 50.7% were mid responders, and 25.4% were high responders.
-
- In the second study 28.6% were low responders, 31.4% were mid responders, and 40% were high responders.
This is a confounding variable for vitamin D studies because the authors of this report estimated:
- Low responders might require 1,25-dihydroxyvitamin D blood levels of 75-100 nmol/L to see a benefit of supplementation. Most studies do not attain 1,25-dihydroxyvitamin D levels that high, so low responders would not appear to benefit from supplementation.
- High responders may already experience optimal benefits of vitamin D at 1,25-dihydroxyvitamin D levels that are generally considered as inadequate. So, supplementation would offer no apparent benefit for this group either.
- Only mid responders might be expected to show a clear benefit from vitamin D supplementation.
The authors concluded, “Individuals can be distinguished into high, mid, and low responders to vitamin D via measuring vitamin D sensitive molecular parameters…Thus, we suggest that the need for vitamin D supplementation depends on the vitamin D status relative to the personal vitamin D response index of an individual rather than on the vitamin D status alone.”
 Report #2 (P Maissan and C Carlberg, Nutrients, 17, 1204, 2025)) suggests that the benefits of vitamin D supplementation might vary depending on the time of day the supplement was taken.
Report #2 (P Maissan and C Carlberg, Nutrients, 17, 1204, 2025)) suggests that the benefits of vitamin D supplementation might vary depending on the time of day the supplement was taken.
This phenomenon is known as circadian rhythm, which describes how time influences physiological and behavioral processes. A little background information is in order.
- We have a “biological clock” that is reset every day by sunlight exposure. Hormone levels rise and physiological processes increase and decrease during the day in response to this biological clock.
- For the most part, you have no knowledge that this is going on in your body but let me share one example you are probably aware of.
-
- Some people suffer from “seasonal affective disorder” (SAD). It is a type of depression associated with the winter months, especially in regions with short days and long nights. For these individuals, bright lights that mimic sunlight are often an effective therapy.
- Some aspects of circadian rhythm are mediated by the pineal gland which produces melatonin. Others are affected by the hypothalamus.
- Since vitamin D synthesis requires sunlight, it makes sense that some vitamin D-responsive genes would also display a circadian rhythm.
This report used the data from the single high-dose vitamin D study described above. They found that:
- Of 361 known vitamin D responsive genes, 87 of them show a clear circadian rhythm.
- For 14 of these genes, there was significant individual variability in the response to vitamin D supplementation.
-
- Group 1 (36% of the population) had significantly higher expression of these genes following vitamin D supplementation than Group 2.
The authors concluded, “Overall, our findings emphasize the circadian nature of vitamin D target gene regulation and highlight interindividual variability in the…responses to vitamin D3 supplementation. These insights have important implications for personalized vitamin D3 supplementation strategies, suggesting that optimal dosing regimens may need to consider both circadian biology [the time of day the supplement is taken] and individual responsiveness to vitamin D.”
What Does This Mean For Clinical Studies?
 The latest reports explain why vitamin D studies are so confusing – why some studies show benefits of vitamin D supplementation and other studies come up empty. Simply put, it’s because vitamin D metabolism is so complicated. Let me walk you through the complications.
The latest reports explain why vitamin D studies are so confusing – why some studies show benefits of vitamin D supplementation and other studies come up empty. Simply put, it’s because vitamin D metabolism is so complicated. Let me walk you through the complications.
1) There is significant individual variability in the conversion of vitamin D to its active 1,25-dihydroxyvitamin D form.
- If vitamin D supplementation does not increase 1,25-dihydroxyvitamin D levels into the adequate range, it is likely that the results will be negative – meaning no benefit of vitamin D supplementation will be observed.
- If 1,25-dihydroxyvitamin D levels are already in the adequate range prior to supplementation, the results may also be negative.
- Fortunately, it is easy to determine blood levels of 1,25-dihydroxyvitamin D in study participants, and most good vitamin D studies are starting to do that.
But vitamin D metabolism just got more complicated. If recent studies are correct:
2) There may be significant individual variability in the biological response to 1,25-dihydroxyvitamin D.
- If someone is a low responder, supplementation at the usual levels of vitamin D is unlikely to result in high enough 1,25-dihydroxyvitamin D levels to give a response.
- If someone is a high responder, they will probably have maxed out their response without supplementation, so adding a vitamin D supplement is unlikely to provide any benefit.
- Sorting participants in clinical studies into low, mid, and high responders is possible, but not easy. Currently the process of sorting individuals into these categories is based on 26 biomarkers. There is no single biomarker that predicts the vitamin D response level for any individual.
3) There may be a circadian rhythm for some beneficial effects of vitamin D. If this observation is confirmed by future research, the time of day vitamin D supplements should be taken may be important.
What Does This Mean For You?
 By this point, you are probably more confused than ever. So, let me sum it up for you.
By this point, you are probably more confused than ever. So, let me sum it up for you.
- Many benefits of vitamin D supplementation are unclear. Some studies show benefits. Others come up empty. “Experts” cherry pick studies that support their beliefs.
- Vitamin D metabolism is complicated. And each new study appears to introduce a new layer of complexity onto our understanding of how vitamin D works.
- Many of the negative vitamin D studies were done before we understood the complexities of vitamin D metabolism or did not take known complexities into account.
- But just because many of the negative studies are flawed doesn’t mean all the claims for vitamin D supplementation are true. Every study has its flaws – both positive and negative studies.
So, here is my advice to you.
#1: Be a cautiously optimistic consumer.
- If your doctor or some internet guru tells you vitamin D supplementation is worthless, don’t believe them. But also, don’t believe claims for miraculous cures with vitamin D supplements.
- We have fairly strong evidence that vitamin D supports healthy bones, a strong immune system, strong muscles, and a healthy brain. If you discover any other benefits of vitamin D supplementation, consider them to be unexpected side benefits.
#2: Base your intake of vitamin D on your blood 1,25-dihydroxyvitamin D levels. The NIH says that 1,25-dihydroxyvitamin D levels of:
- <30 nmol/L indicate vitamin D deficiency
- 30 to <50 nmol/L indicate vitamin D insufficiency.
- >50 nmol/L are adequate.
- >125 nmol/L may be linked to adverse effects.
#3: Because you don’t know whether you are a low, mid, or high responder to 1,25-dihydroxyvitamin D, you may want to shoot for a 1,25-dihydroxyvitamin D level of somewhat greater than 50 nmol/L (the study said that low responders may need as much as 75-100 nmol/L).
- Personally, I would aim for no more than 60-80 nmol/L because I would not want to risk vitamin D toxicity. I realize that 125 nmol/L is the lower limit set for toxicity, but I prefer to err on the side of caution.
#4: Be aware that there may be a circadian rhythm to the effectiveness of your vitamin D supplement.
- Sunlight is required for synthesis of vitamin D. So, if there is a circadian rhythm to vitamin D effectiveness, vitamin D supplements might be more effective if taken in the morning than at night.
The Bottom Line
Why do so many studies on the benefits of vitamin D supplementation come up empty? Perhaps it’s because many investigators don’t understand the complexities of vitamin D metabolism. For example:
1) There is significant individual variability in the conversion of vitamin D to its active 1,25-dihydroxyvitamin D form.
- This has been well characterized, and the best vitamin D studies are starting to incorporate 1,25-dihydroxyvitamin D measurements into their study design.
And recent studies have added to the complexity of vitamin D metabolism. Our understanding of vitamin D just got a lot more complicated. For example, these studies suggest that:
2) There may be significant individual variability in the biological response to 1,25-dihydroxyvitamin D levels.
3) There may be a circadian rhythm for some beneficial effects of vitamin D.
- These observations have yet to be incorporated into clinical studies of vitamin D supplementation and may explain why some existing studies have failed to find beneficial effects of vitamin supplementation.
For more details on these studies and what they may mean for you, read the article above.
These statements have not been evaluated by the Food and Drug Administration. This information is not intended to diagnose, treat, cure or prevent any disease.
______________________________________________________________________________
My posts and “Health Tips From the Professor” articles carefully avoid claims about any brand of supplement or manufacturer of supplements. However, I am often asked by representatives of supplement companies if they can share them with their customers.
My answer is, “Yes, as long as you share only the article without any additions or alterations. In particular, you should avoid adding any mention of your company or your company’s products. If you were to do that, you could be making what the FTC and FDA consider a “misleading health claim” that could result in legal action against you and the company you represent.
For more detail about FTC regulations for health claims, see this link.
https://www.ftc.gov/business-guidance/resources/health-products-compliance-guidance
_______________________________________________________________________
About The Author
 Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney has a BS in Chemistry from Duke University and a PhD in Biochemistry from UCLA. He is Professor Emeritus from the University of North Carolina where he taught biochemistry and nutrition to medical and dental students for 40 years.
Dr. Chaney won numerous teaching awards at UNC, including the Academy of Educators “Excellence in Teaching Lifetime Achievement Award”.
Dr Chaney also ran an active cancer research program at UNC and published over 100 scientific articles and reviews in peer-reviewed scientific journals. In addition, he authored two chapters on nutrition in one of the leading biochemistry text books for medical students.
Since retiring from the University of North Carolina, he has been writing a weekly health blog called “Health Tips From the Professor”. He has also written two best-selling books, “Slaying the Food Myths” and “Slaying the Supplement Myths”. And most recently he has created an online lifestyle change course, “Create Your Personal Health Zone”. For more information visit https://chaneyhealth.com.
For the past 53 years Dr. Chaney and his wife Suzanne have been helping people improve their health holistically through a combination of good diet, exercise, weight control and appropriate supplementation.




